Mississippi Today
'You're not in line': Family battles politics, indifference, and suspected fraud in federal health care program
‘You’re not in line’: Family battles politics, indifference, and suspected fraud in federal health care program
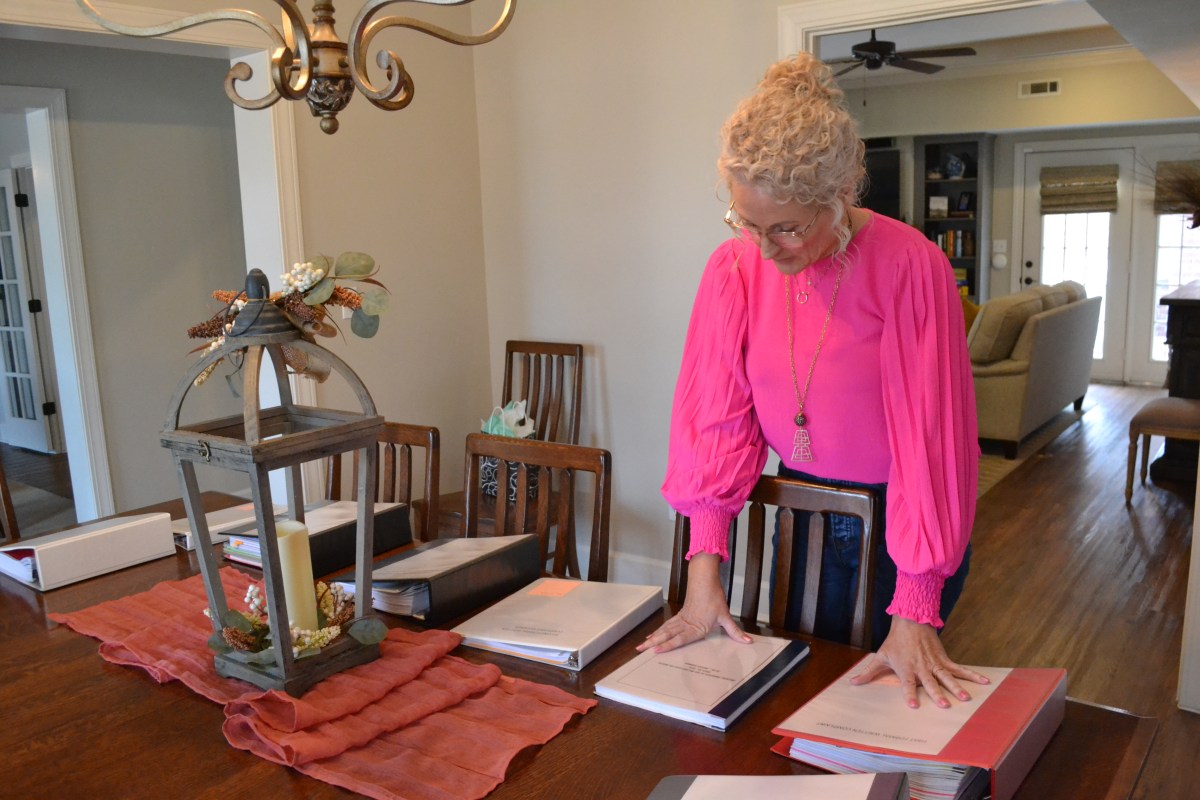
Natalie Gunnells had finally secured some assistance from Mississippi’s political class for her 23-year-old son Patrick, who has severe autism.
No sooner had she started receiving relief from the state’s Medicaid agency than her local lawmaker accused her of supporting his political opponent, delivering an ominous warning.
“You’re not in line, you’re not in sync to help you and your family,” said the local senator.
Patrick is one of 2,750 Mississippians on a special Medicaid program that is supposed to provide outpatient services to people with intellectual or developmental disabilities, known as the IDD waiver. The purpose of the waiver — a roughly $125 million-a-year program funded mostly by the federal government but administered by state agencies — is to allow this vulnerable population to live in the community as opposed to an inpatient facility.
But even though he receives the waiver, Patrick has for years lacked a caregiver or specialist.
“I’m telling you this waiver is designed to fail. You don’t fail this many people year, after year, after year if it is not designed to fail,” Natalie Gunnells said at a community meeting in February.
Without the specialized behavioral therapy that he is eligible to receive, Patrick’s potential is unknown. Patrick is nonverbal and cannot perform normal tasks, like using the bathroom on his own. When he was a child, his parents fought for him to receive the special education he was entitled to at the public school. These days, Patrick rarely agrees to leave the family’s Tupelo home, and he’s almost always wearing his large black headphones due to noise sensitivity.
Yet, the Gunnells recently found out that Medicaid has been dishing out thousands for therapy they say Patrick is not receiving under what they believe is a fraud scheme. Documents suggest the alleged abuse was made possible by years of loose oversight at the Department of Mental Health. The state attorney general’s office is currently investigating, according to AG communication obtained by Mississippi Today, though no one has been charged with a crime.
READ MORE: Attorney General investigating provider fraud in Medicaid waiver

Adding insult to injury, when the federal government decided during the pandemic to temporarily allow parents to get paid to deliver care to their disabled adult children, Mississippi chose not to adopt the policy.
Natalie Gunnells and her husband Jamie Gunnells knew they’d have to involve Sen. Chad McMahan, R-Guntown, their local lawmaker, if they wanted a shot at the new benefit.
It was the same way when Patrick got on the waiver, known for its years-long waitlist, more than a decade ago.
“You have to know somebody to get off the waiting list,” said Jamie Gunnells, who owns and runs an independent pharmacy in Tupelo. “It’s pitiful.”
In roughly the last year, Mississippi Division of Medicaid Director Drew Snyder asked one of his division directors to follow up on requests from at least eight sitting lawmakers, all white Republican men, according to text messages obtained by Mississippi Today. The politicians seemed to urge the agency to remove roadblocks for specific beneficiaries who were attempting to access Medicaid.
In each case, Tracy Buchanan, Medicaid’s director of long term services and supports, responded that she was on it.
READ MORE: Texts show lawmaker influence over Mississippi’s Medicaid rolls
McMahan has become particularly known for keenly navigating government red tape to help Mississippians get the public assistance they need. “I am relentless about contacting these agencies on my own,” McMahan told Mississippi Today. “I personally call and take an interest in every one of these cases to help people.”
As part of his stated commitment to help his constituents, McMahan convened a meeting for the Gunnells with Medicaid officials in May of 2022. After it ended, the couple alleged that McMahan casually propositioned them.
“He says, ‘Well, that ought to be worth a $25,000 campaign donation, don’t you think?’” Jamie Gunnells said.

While the Gunnells, who have publicly shared support for various Mississippi politicians, had made contributions to McMahan’s past campaigns, they said they were put off by the request and have not donated to McMahan since.
McMahan adamantly denied making the ask for a campaign donation. “No, I didn’t say anything like that,” he said. “… That’s a terrible thing to say.”
In Mississippi, it’s not uncommon for the state’s Republican leaders, who otherwise revile public assistance programs, to use the system for the benefit of themselves and their political supporters — no better illustrated than within Mississippi’s still-unfolding welfare scandal. One former grant recipient and defendant in the case, Christi Webb, even accused McMahan of delivering a threat on behalf of former Gov. Phil Bryant to withhold grant funding to the nonprofit she ran, Family Resource Center of North Mississippi, because she had supported and hired the wife of a Democratic candidate for governor. McMahan denied the allegation.
McMahan had also been jockeying for funding from Mississippi Department of Human Services, which administers the federal Temporary Assistance to Needy Families (TANF) block grant, to go to the Autism Center of North Mississippi. For a short time years ago, Patrick received services from the autism center, and his parents praised the quality of the program.
Auditors found that the autism center improperly received a $75,000 grant from the welfare agency, as well as more than $300,000 in grants from Family Resource Center.
MDHS employees had expressed hesitation about whether anti-poverty funds could be used to support services for well-to-do families at the autism center, but after a meeting between McMahan, Bryant and the welfare director, grant money flowed to the center anyway.

At the Gunnells’ urging, the Mississippi Division of Medicaid eventually adopted the federal policy allowing parents of severely disabled adults to temporarily become paid caregivers.
Natalie Gunnells, who has a master’s degree in counseling and gave up a promising career in education to care for her son, took courses to become certified through a local personal care provider last year.
Still, Mississippi had chosen the more stringent version of the policy that said legal guardians could not participate. So Natalie Gunnells had to relinquish her guardianship of Patrick — at a price of $2,300 to her attorney — to serve as her son’s taxpayer-funded caregiver. She began receiving the $12-an-hour wage for her work in November. This temporary policy, called Appendix K, only lasts until the end of the public health emergency, currently planned for next month.
In early January, Natalie Gunnells shared what she thought was an innocuous Facebook post from Lauren Smith, a local lab tech consultant and growing social media personality. Smith promotes conservative politics through her Facebook group “P.R.I.M.E” (Patriots for Rights Integrity Morals and Ethics), often taking aim at establishment GOP leaders. She was gearing up to run against McMahan for his Senate seat.
“If you want to know what’s really going on in politics in our great State, then you need to listen to Lauren Smith!” Natalie Gunnells wrote. “Ya’ll, this girl…her passion, knowledge, expertise…JUST LISTEN!”
Then her phone rang.
On the other line, McMahan explained to the Gunnells that “someone in Washington” had alerted him to Natalie Gunnell’s Facebook post, and they weren’t happy.
“There’s some of us out here that are doing everything we can to help your family, and it’s just, it’s just a slap in our face,” McMahan said, according to a recording of the call obtained by Mississippi Today. “… I just want you to know that I may be the face of trying to help you, but there’s a lot of people behind me that’s tried to help you, and y’all are making it difficult for your own cause.”
“We’re making it difficult by liking a post?” Jamie Gunnells said.
“Yes,” McMahan said. “Yes.”
“I don’t understand that,” Jamie said.
“Well, I guess you’ll just have to trust me. I don’t know the pharmaceutical industry, but I know politics. And I guess you’ll just have to trust me,” the lawmaker said, according to the recording.
To the Gunnells, McMahan’s call came off as a veiled threat to withhold help to Patrick.
“That’s terrible. If that’s the impression I left, I’m really, I’m deeply sorry about that,” McMahan told Mississippi Today. “I thought they would deceive my sincerity about how hard I had worked on their behalf, and they know I did.”
But on the call, McMahan also accused his opponent of wanting to end Medicaid — the program that provides not only Patrick’s waiver, but his health insurance. “She (Smith) is against every type of program,” McMahan told the Gunnells. “She would take literally the bread out of your family’s mouth to end any type of government assistance, and you’re supporting her.”
After the interaction, Natalie Gunnells said she felt that the solution they had reached with Medicaid was in jeopardy. She deleted her Facebook post.
“Senator McMahan was referring to a quid pro quo: he was helping us and if we wanted to continue to rely on him and everyone he stated behind him helping, we better not promote Lauren Smith at all,” Natalie Gunnells wrote to Mississippi Today.
McMahan explained his response to the situation, telling Mississippi Today, “It’s a normal reaction when you help somebody and then they’re out there supporting other individuals that are completely opposed to their own need.”
“It is human nature. I mean, come on,” he told Mississippi Today. “You give somebody just hours and hours of help in trying to help their family, and then they’re out there supporting individuals, not just my opponent, but other individuals in general that are against any type of Medicaid enhancements. And it’s just odd.”

The Gunnells are ardent conservatives, backing far-right candidates such as Sen. Chris McDaniel, a Republican candidate for lieutenant governor and tea party populist who’s tried to fracture Mississippi’s establishment GOP since at least his U.S. Senate race in 2014. These candidates are particularly hostile to taxpayer spending on government assistance programs.
But the Gunnells said they don’t believe Smith or any other public servant would genuinely want to eliminate Medicaid.
“I can’t imagine a politician saying that today,” Jamie Gunnells said. “Yeah, they and I would love to see more people working and supporting themselves, but we’re the poorest state in the union, we’re going to have people on Medicaid. And that’s just the fact.”
Smith told Mississippi Today that McMahan, who also filed an unsuccessful residency challenge against Smith, is desperate to hold onto his senate seat, “and he’ll say whatever it takes to do that, no matter if it’s true or a lie.”
“Do I think it (Medicaid) needs reforming? Absolutely. Do I think it is a very, very broken system? Absolutely. And it does need a lot of work. But to do away with it? No, absolutely not,” Smith said. “It’s there for a reason, and that’s to take care of the ones who truly need it.”
Smith also said she is against the extension of postpartum Medicaid coverage from 60 days to one year, which Gov. Tate Reeves recently signed into law.
“Why is that a Mississippi taxpayer’s problem to have to pay for that?” Smith said. “… Whenever I had my son, I had to go back to work.”
At least 40% of private sector jobs in Mississippi do not come with employer-sponsored health benefits, according to Kaiser Family Foundation.
Regardless of the state’s philosophy around Medicaid, its administration of the IDD waiver has been a disaster, according to several parents who spoke at a public hearing in February. This is largely because of a shortage of quality direct care workers and shoddy oversight.
Medicaid is responsible for submitting a renewal application to the federal government every five years to keep the waiver in operation. It held a hearing to gather feedback from clients in February and sent the new waiver application at the end of March.
The purpose of the waiver is to allow people with intellectual and developmental disabilities to live in the community, as opposed to an inpatient facility. This follows the 1999 U.S. Supreme Court opinion in Olmstead v.s L.C., which gives Americans with disabilities the right to live in the “least restrictive setting” possible for their condition and requires the government to provide the necessary supports.
While there are about 2,750 people on the waiver at any given time, there are almost the same number of people on the waiting list who qualify but do not get the benefit. The state estimates there are a total of between 52,000 to 53,000 Mississippians with intellectual or developmental disabilities.
“People are being institutionalized, I firmly believe, because they can’t get on the waiver,” said Polly Tribble, director of Disability Rights Mississippi.
Around 700 people with intellectual and developmental disabilities live in the state’s six regional facilities. This is down from roughly 1,300 residents in 2012. The IDD waiver has grown in that time from about 1,800 to more than 2,700.
Tribble’s largest concern within the waiver is how few people it serves. She told the story of a mother who had to put her daughter in an institution because she couldn’t afford to give up her job to stay home.
“She was separated from her daughter for years until we found out about it and got her some help,” Tribble said. “There’s stories like that all across the state. We don’t know what the potential is and you’re talking about somebody’s quality of life. And possibly somebody’s life.”
But the waiver doesn’t necessarily ensure a person will receive the services they need.
“If you think this is going to be a golden ticket, it’s not,” Natalie Gunnells said.
Every morning, the Gunnells trade off who is responsible for getting Patrick up, bathing him, getting him dressed, and feeding him breakfast. After that, Natalie Gunnells is almost always at home tending to Patrick, helping him go to the bathroom and bringing him meals.
The highlight of Patrick’s day is when his 16-year-old brother Stephen gets back from school. The rest of their four siblings, ages 21 to 27, no longer live at home.
In addition to a primary diagnosis of autism, Patrick also has a genetic disorder called Cri-du-chat. But while his capabilities are limited, Patrick is smart; he can read books on at least a 9th grade level and communicate through a speech-generating device.
Patrick qualifies for 180 hours per month of in-home respite care, which is designed to relieve a primary caregiver of their otherwise round-the-clock work. For six of the last seven years, his mom said Patrick has been without a respite caregiver.
Not every person on the IDD waiver may need in-home respite, though all would qualify for it. Out of the 2,747 people on the waiver in fiscal year 2022, less than 20%, or 534, received respite care, according to documents from Medicaid. Just 32%, 873, received a similar service called home and community supports.
Patrick can’t participate in community-based services in centers, often referred to as day hab, because DMH doesn’t fund the one-on-one support he would need to acclimate in that environment.
Patrick also qualifies for 30 hours of behavioral therapy each month. Natalie Gunnells said that a local behavior support consultant, Vargas Clark from Mississippi Behavioral Services, did come to the Gunnells’ home to work with Patrick here and there in 2018, only for around 30 minutes a session. But they say Clark hasn’t had much of a presence in their lives since, and while a different therapist from the Behavioral Services came sporadically in 2021, the Gunnells haven’t seen anyone from the organization in over a year.
According to Medicaid’s billing department, the IDD waiver costs about $125 million annually, with the agency reimbursing about $45,000 worth of services on average for each person on the waiver – though clients like Patrick aren’t receiving nearly that amount.
Some parents who spoke to Mississippi Today are skeptical, considering the worker shortage, that such a large amount of care or therapy is actually being delivered under the waiver.
“They’re receiving funding, but the services are not being delivered as they are designed to be,” Deb Giles, a parent of a son with Down syndrome, said at a recent hearing.
If Natalie Gunnells were paid to provide Patrick’s full allotment of in-home care, it would cost roughly $25,000 each year. To compare, the cost of placing Patrick in one of DMH’s regional centers would be anywhere from $90,000 to $170,000 a year depending on the level of care he qualified for.
The waiver is funded by Medicaid but the administration and oversight, which primarily consists of support coordinators employed by the regional IDD centers, is operated by the Mississippi Department of Mental Health. DMH told Mississippi Today that like private direct care providers, the agency has similarly struggled to hire and retain enough support coordinators.
The support coordinators work with the IDD waiver clients and their parents or guardians to develop what’s called a Plan of Services and Supports. The plan, the state’s primary source of information about how a patient is faring, is a crude worksheet with blank spaces for the support coordinator to fill out. Some of the headers include, “Things People Need to Know to Support Patrick and Keep Patrick Safe,” “Patrick’s Strengths,” “Patrick’s Dreams,” “Things to Figure Out,” “Good Day,” and “Bad Day.”
At least in Patrick’s case, the plan operates as more of a wishlist than a realistic picture of his participation in the program. In some cases, it seems to the Gunnells that DMH is simply checking boxes, even if that means jotting down inaccuracies. The Gunnells’ support coordinator, Clay Ketchings at North Mississippi Regional Center, repeatedly writes in the plan that Patrick likes to go on car rides, despite the fact that currently, his parents say Patrick is almost entirely homebound.
Ideally, the Gunnells would find a consistent direct care worker and use the behavior support consultant to train the worker on how to best socialize and respond to Patrick’s specific needs. Patrick’s waiver plan explains that he is stubborn to following directions, sometimes falling on the ground and refusing to move. The Gunnells wonder what Patrick would be capable of if he had access to an autism specialist, especially considering the promising progress he made during the short stint he received services from the autism center under Dr. Sheila Williamson, who’s no longer there.
“She would have probably already had him potty trained,” Natalie Gunnells said. “… So we don’t ever really know what his potential is.”
In Mississippi, there are almost two direct care worker job openings for every person working as a direct care worker, according to national policy institute PHI, which ranks Mississippi second to last for its direct care workforce.
Betty Pinion, director of the IDD program for the Department of Mental Health, acknowledged the care shortage in an interview with Mississippi Today. But she also said that in some cases, individuals on the waiver are not receiving the services included in their plan not because the services aren’t available, but because the family refuses to work with the available providers. Some of these agencies are paying direct care workers as low as $8-an-hour.
“There are some (clients) that doesn’t seem to be satisfied with any person that we send,” Pinion said.
Since the Gunnells haven’t found a direct care worker to train, they haven’t been receiving the behavioral support either.
They and many other parents have raised the issue of lack of services to their support coordinator, who is tasked with addressing any client concerns, but they say it doesn’t yield any results. Mississippi Today observed one family’s Plan of Services and Supports meeting in March. The parents repeatedly complained that they could not find an agency with available workers; the support coordinator explained that she didn’t have any control over the workforce.
In an interview with Mississippi Today, officials from the Department of Mental Health said it is not tracking how many people on the waiver are receiving each service versus the number of people eligible for each service.
This could show the number of people missing out on the benefits to which they’re entitled.
It also does not compile the total number of hours per service people on the waiver are eligible to receive or the total number of hours of services delivered, which might even better quantify the care shortage. Mississippi Today requested this data from the department, but since it is not already compiled in a report, it is not a public record, and the department said the report would require too many hours for the agency to conduct.
“To compile the requested information, each individual’s file (more than 2,700) would have to be reviewed to determine the eligible number of hours and then compiled into a consolidated report,” the agency said in response to the request. “… DMH is considering ways this data can be collected in the future.”
Medicaid declined to answer Mississippi Today’s questions about the waiver and its renewal, but an attorney with the agency Cody Smith told Natalie Gunnells in an email that the agency shared her concerns about the care shortage. He said that Medicaid is working with DMH to “lower barriers on workers entering the industry” and that it has commissioned a workforce study. Medicaid spokesperson Matt Westerfield said the agency is proposing an average reimbursement rate increase of 18%, which affects the hourly wage of the care workers.
Medicaid is currently submitting its paperwork to the federal government to renew the IDD waiver, a process that happens once every five years. Both Medicaid and DMH hosted a public hearing in February to accept suggestions from the public about what changes to make in its renewal.
After Mississippi Today’s inquiry to Medicaid about the IDD waiver, Snyder texted his deputy administrator for policy Wil Ervin, who recently left the agency, asking him to watch a recording of the public hearing to see if there was anything they needed to “watch out for.”
“We are likely going to have an issue from the hearing,” Ervin responded the next day.
Medicaid spokesperson Matt Westerfield said in an email that Ervin was referring to complaints, such as from Natalie Gunnells, about the policy that legal guardians cannot be paid caregivers under the waiver. Westerfield said last month that the agency was still considering whether to revise this policy in its permanent plan.
But when it came time to submit the waiver application at the end of March, Medicaid moved to include an even more restrictive version of the policy. It added the caveat that people could not be paid to care for their relatives if the service they are providing is “a function that a relative or housemate was providing for the participant without payment prior to waiver enrollment,” which seems to apply to Natalie Gunnells and most parents in her position.
After all her efforts, Natalie Gunnells will likely be back at square one when the public health emergency ends.

In early January of 2022, frustrated by the absence of services for her son, Natalie Gunnells began requesting what are called “utilization reports” from the Department of Mental Health.
The reports contain which services, and the number of hours, that providers are billing to Medicaid under the waiver. The support coordinators are supposed to review the documents with the parent or guardian every month to ensure the client is receiving the services that Medicaid is paying for, but in Natalie Gunnells’s case, she said this hadn’t happened for three years.
“They were so negligent that any agency billing Medicaid that wanted to commit fraud could without detection,” Natalie Gunnells wrote in her own timeline of the alleged fraud.
Once she got the documents, she said she realized that for at least two years, Mississippi Behavioral Services, owned by Vargas Clark in Southaven, had been charging Medicaid for services she says Patrick wasn’t receiving. In some months when Patrick may have received an hour of support, billing records show the company charged for the full 30 hours. Natalie Gunnells estimates Medicaid reimbursed Mississippi Behavioral Services for at least $42,000 for services not rendered.
Clark, who has not been charged with a crime, told Mississippi Today Monday that he was unaware of an investigation into his company. After agreeing to examine his records in order to discuss the alleged billing discrepancies, he did not return several follow up calls or texts.
Natalie Gunnells reported her findings to Medicaid’s fraud division, but she said they never responded. She then took the information to the Attorney General’s Office, which launched an investigation, in September. The Gunnells submitted an affidavit in October. The AG did not respond to several requests for comment for this story. DMH confirmed that it conducted its own internal investigation and referred the matter to Medicaid. DMH Director Wendy Bailey also said the agency recently provided more training to support coordinators to ensure they’re following procedures.
Providers are supposed to submit quarterly review reports describing the patient’s progress, but the Gunnells’ support coordinator hadn’t been collecting them from Mississippi Behavioral Services.
Eventually, Natalie Gunnells got the records from the investigator. According to a review by Mississippi Today, many of the reports are identical from quarter to quarter, seemingly copy-pasted with only the date at the top changing. The investigator also shared invoices and billing records from Medicaid, some of which include signatures for Natalie Gunnells that she said aren’t hers and indistinguishable scribbles for the others.
The reviews include charts, lines zigzagging across the page, that pretend to reflect the frequency of Patrick’s “target behaviors,” such as noncompliance and physical aggression. As far as Natalie Gunnells is concerned, the data is made up.
“Patrick has shown a positive response to behavior treatment,” one report says, referencing a three-month period in which the Gunnells say no therapist ever came to see Patrick.
This article first appeared on Mississippi Today and is republished here under a Creative Commons license.
Mississippi Today
Hospitals see danger in Medicaid spending cuts
Mississippi hospitals could lose up to $1 billion over the next decade under the sweeping, multitrillion-dollar tax and policy bill President Donald Trump signed into law last week, according to leaders at the Mississippi Hospital Association.
The leaders say the cuts could force some already-struggling rural hospitals to reduce services or close their doors.
The law includes the largest reduction in federal health and social safety net programs in history. It passed 218-214, with all Democrats voting against the measure and all but five Republicans voting for it.
In the short term, these cuts will make health care less accessible to poor Mississippians by making the eligibility requirements for Medicaid insurance stiffer, likely increasing people’s medical debt.
In the long run, the cuts could lead to worsening chronic health conditions such as diabetes and obesity for which Mississippi already leads the nation, and making private insurance more expensive for many people, experts say.
“We’ve got about a billion dollars that are potentially hanging in the balance over the next 10 years,” Mississippi Hospital Association President Richard Roberson said Wednesday during a panel discussion at his organization’s headquarters.
“If folks were being honest, the entire system depends on those rural hospitals,” he said.
Mississippi’s uninsured population could increase by 160,000 people as a combined result of the new law and the expiration of Biden-era enhanced subsidies that made marketplace insurance affordable – and which Trump is not expected to renew – according to KFF, a health policy research group.
That could make things even worse for those who are left on the marketplace plans.
“Younger, healthier people are going to leave the risk pool, and that’s going to mean it’s more expensive to insure the patients that remain,” said Lucy Dagneau, senior director of state and local campaigns at the American Cancer Society.
Among the biggest changes facing Medicaid-eligible patients are stiffer eligibility requirements, including proof of work. The new law requires able-bodied adults ages 19 to 64 to work, do community service or attend an educational program at least 80 hours a month to qualify for, or keep, Medicaid coverage and federal food aid.
Opponents say qualified recipients could be stripped of benefits if they lose a job or fail to complete paperwork attesting to their time commitment.
Georgia became the case study for work requirements with a program called Pathways to Coverage, which was touted as a conservative alternative to Medicaid expansion.
Ironically, the 54-year-old mechanic chosen by Georgia Gov. Brian Kemp to be the face of the program got so fed up with the work requirements he went from praising the program on television to saying “I’m done with it” after his benefits were allegedly cancelled twice due to red tape.
Roberson sent several letters to Mississippi’s congressional members in weeks leading up to the final vote on the sweeping federal legislation, sounding the alarm on what it would mean for hospitals and patients.
Among Roberson’s chief concerns is a change in the mechanism called state directed payments, which allows states to beef up Medicaid reimbursement rates – typically the lowest among insurance payors. The new law will reduce those enhanced rates to nearly as low as the Medicare rate, costing the state at least $500 million and putting rural hospitals in a bind, Roberson told Mississippi Today.
That change will happen over 10 years starting in 2028. That, in conjunction with the new law’s one-time payment program called the Rural Health Care Fund, means if the next few years look normal, it doesn’t mean Mississippi is safe, stakeholders warn.
“We’re going to have a sort of deceiving situation in Mississippi where we look a little flush with cash with the rural fund and the state directed payments in 2027 and 2028, and then all of a sudden our state directed payments start going down and that fund ends and then we’re going to start dipping,” said Leah Rupp Smith, vice president for policy and advocacy at the Mississippi Hospital Association.

Even with that buffer time, immediate changes are on the horizon for health care in Mississippi because of fear and uncertainty around ever-changing rules.
“Hospitals can’t budget when we have these one-off programs that start and stop and the rules change – and there’s a cost to administering a program like this,” Smith said.
Since hospitals are major employers – and they also provide a sense of safety for incoming businesses – their closure, especially in rural areas, affects not just patients but local economies and communities.
U.S. Rep. Bennie Thompson is the only Democrat in Mississippi’s congressional delegation. He voted against the bill, while the state’s two Republican senators and three Republican House members voted for it. Thompson said in a statement that the new law does not bode well for the Delta, one of the poorest regions in the U.S.
“For my district, this means closed hospitals, nursing homes, families struggling to afford groceries, and educational opportunities deferred,” Thompson said. “Republicans’ priorities are very simple: tax cuts for (the) wealthy and nothing for the people who make this country work.”
While still colloquially referred to as the One Big Beautiful Bill Act, the name was changed by Democrats invoking a maneuver that has been used by lawmakers in both chambers to oppose a bill on principle.
“Democrats are forcing Republicans to delete their farcical bill name,” Senate Democratic Leader Charles Schumer of New York said in a statement. “Nothing about this bill is beautiful — it’s a betrayal to American families and it’s undeserving of such a stupid name.”
The law is expected to add at least $3.3 trillion to the nation’s debt over the next 10 years, according to the most recent estimate from the Congressional Budget Office.
This article first appeared on Mississippi Today and is republished here under a Creative Commons Attribution-NoDerivatives 4.0 International License.
The post Hospitals see danger in Medicaid spending cuts appeared first on mississippitoday.org
Note: The following A.I. based commentary is not part of the original article, reproduced above, but is offered in the hopes that it will promote greater media literacy and critical thinking, by making any potential bias more visible to the reader –Staff Editor.
Political Bias Rating: Center-Left
This article reports on the negative impacts of a major federal tax and policy bill on Medicaid funding and rural hospitals in Mississippi. While it presents factual details and statements from stakeholders, the tone and framing emphasize the harmful consequences for vulnerable populations and health care access, aligning with concerns typically raised by center-left perspectives. The article highlights opposition by Democrats and critiques the bill’s priorities, particularly its effect on poor and rural communities, suggesting sympathy toward social safety net preservation. However, it maintains mostly factual reporting without overt partisan language, resulting in a moderate center-left bias.
Crooked Letter Sports Podcast
Podcast: The Mississippi Sports Hall of Fame Class of ’25
The MSHOF will induct eight new members on Aug 2. Rick Cleveland has covered them all and he and son Tyler talk about what makes them all special.
Stream all episodes here.
This article first appeared on Mississippi Today and is republished here under a Creative Commons Attribution-NoDerivatives 4.0 International License.
The post Podcast: The Mississippi Sports Hall of Fame Class of '25 appeared first on mississippitoday.org
Mississippi Today
‘You’re not going to be able to do that anymore’: Jackson police chief visits food kitchen to discuss new public sleeping, panhandling laws
Diners turned watchful eyes to the stage as Jackson Police Chief Joseph Wade took to the podium. He visited Stewpot Community Services during its daily free lunch hour Thursday to discuss new state laws, which took effect two days earlier, targeting Mississippians experiencing homelessness.
“I understand that you are going through some hard times right now. That’s why I’m here,” Wade said to the crowd. “I felt it was important to come out here and speak with you directly.”
Wade laid out the three bills that passed earlier this year: House Bill 1197, the “Safe Solicitation Act,” HB 1200, the “Real Property Owners Protection Act” and HB 1203, a bill that prohibits camping on public property.
“Sleeping and laying in public places, you’re not going to be able to do that anymore,” he said. “There’s a law that has been passed that you can’t just set up encampments on public or private properties where it’s a public nuisance, it’s a problem.”
The “Real Property Owners Protection Act,” authored by Rep. Brent Powell, R-Brandon, is a bill that expedites the process of removing squatters. The “Safe Solicitation Act,” authored by Rep. Shanda Yates, I-Jackson, requires a permit for panhandling and allows people to be charged with a misdemeanor if they violate this law. The offense is punishable by a fine not to exceed $300 and an offender could face up to six months in jail. Wade said he’s currently working with his legal department to determine the best strategy for creating and issuing permits.
“We’re going to navigate these legal challenges, get some interpretations, not only from our legal department, but the Attorney General’s office to ensure that we are doing it legally and lawfully, because I understand that these are citizens,” he said. “I understand that they deserve to be treated with respect, and I understand that we are going to do this without violating their constitutional rights.”
Wade said the Jackson Police Department is steadily fielding reports of squatters in abandoned properties and the law change gives officers new power to remove them more quickly. The added challenge? Figuring out what to do with a person’s belongings.
“These people are carrying around what they own, but we are not a repository for all of their stuff,” he said. “So, when we make that arrest, we’ve got to have a strategic plan as to what we do with their stuff.”
Wade said there needs to be a deeper conversation around the issues that lead someone to becoming homeless.
“A lot of people that we’re running across that are homeless are also suffering from medical conditions, mental health issues, and they’re also suffering from drug addiction and substance abuse. We’ve got to have a strategic approach, but we also can’t log jam our jail down in Raymond,” Wade said.
He estimates that more than 800 people are currently incarcerated at the Raymond Detention Center, and any increase could strain the system as the laws continue to be enforced.
“I think there’s layers that we have to work through, there’s hurdles that we are going to overcome, but we’ve got to make sure that we do it and make sure that my team and JPD is consistent in how we enforce these laws,” Wade said.
Diners applauded Wade after he spoke, in between bites of fried chicken, salad, corn and 4th of July-themed packaged cakes. Wade offered to answer questions, but no one asked any.
Rev. Jill Buckley, executive director of Stewpot, said that the legislation is a good tool to address issues around homelessness and community needs. She doesn’t want to see people who are homeless be criminalized, but she also wants communities to be safe.
“I support people’s right to self determine, and we can’t impose our choices on other people, but there are some cases in which that impinges on community safety, and so to the extent that anyone who is camping or panhandling or squatting and is a danger to themselves and others, of course, I fully support that kind of law. I don’t support homelessness being criminalized as such,” Buckley said.

Many of the people Wade addressed while they ate Thursday said they have housing, don’t panhandle, and shouldn’t be directly impacted by the legislation. But Marcus Willis, 42, said it would make more sense if elected officials wanted to combat the negative impacts of homelessness that they help more people secure employment.
“There ain’t enough jobs,” said Willis, who was having lunch with his girlfriend Amber Ivy.
The two live in an apartment together nearby on Capitol Street, where Ivy landed after her mother, whom Ivy had been living with, suffered a stroke and lost the property. Similarly, Willis started coming to eat at Stewpot after his grandmother, whose house he used to visit for lunch, passed away.
Willis holds odd jobs – cutting grass, home and auto repair – so the income is inconsistent, and every opportunity for stable employment he said he’s found is outside of Jackson in the suburbs. The couple doesn’t have a car.
Making rent every month usually depends on their ability to find someone to help chip in, said Ivy, who is in recovery from substance abuse. She said she’s watched problems surrounding homelessness grow over the years in Jackson. Ivy grew up near Stewpot and has lived in various neighborhoods across the city – except for the times she moved out of state when things got too rough.
“There was just moments where I just had to leave,” Ivy said. “Sometimes if you hit a slump here, there’s almost no way for you to get out of it.”
This article first appeared on Mississippi Today and is republished here under a Creative Commons Attribution-NoDerivatives 4.0 International License.
The post 'You're not going to be able to do that anymore': Jackson police chief visits food kitchen to discuss new public sleeping, panhandling laws appeared first on mississippitoday.org
Note: The following A.I. based commentary is not part of the original article, reproduced above, but is offered in the hopes that it will promote greater media literacy and critical thinking, by making any potential bias more visible to the reader –Staff Editor.
Political Bias Rating: Center-Right
This article primarily reports on new laws in Jackson, Mississippi, targeting public sleeping, panhandling, and squatting, focusing on statements by Police Chief Joseph Wade and community perspectives. The coverage presents the legislative measures—authored by Republican and independent lawmakers—with a tone that emphasizes law enforcement challenges and community safety, reflecting a conservative approach to homelessness as a public order issue. While it includes voices concerned about criminalization and the need for social support, the overall framing centers on law enforcement and property protection. The article maintains factual reporting without overt editorializing but leans slightly toward a center-right perspective by highlighting legal enforcement as a solution.
-
News from the South - Arkansas News Feed6 days ago
Real-life Uncle Sam's descendants live in Arkansas
-
News from the South - Georgia News Feed5 days ago
'Big Beautiful Bill' already felt at Georgia state parks | FOX 5 News
-
News from the South - Oklahoma News Feed6 days ago
LOFT report uncovers what led to multi-million dollar budget shortfall
-
News from the South - Alabama News Feed7 days ago
Alabama schools to lose $68 million in federal grants under Trump freeze
-
News from the South - Missouri News Feed7 days ago
Celebrate St. Louis returns with new Superman-themed drone show
-
News from the South - South Carolina News Feed7 days ago
South Carolina lawmakers react as House approves Trump’s sweeping economic package
-
Local News6 days ago
Maroon Tide football duo commits to two different SEC Teams!
-
News from the South - North Carolina News Feed5 days ago
Raleigh caps Independence Day with fireworks show outside Lenovo Center