Matt Bird/Stone via Getty Images
Steven R. Fassnacht, Colorado State University
It’s extremely easy to get sunburned while you’re skiing and snowboarding in the mountains, but have you ever wondered why?
While it’s true that you’re slightly closer to the Sun when you’re high in the mountains, that isn’t the reason.
If you go up 1 mile (1.6 km), about the elevation from Denver to the peaks of resorts such as Vail or Copper Mountain, you’re less than 1 millionth of a percent closer to the Sun – that’s nothing. Since the Earth’s orbit is an ellipse and not a circle, the planet is about 1.7% closer to the Sun in early January compared with its annual average. This means skiers get about 3.3% more Sun in January than average for the year – so, not much more.
Being 1 mile higher up does mean the atmosphere is thinner, so there are fewer particles to block the ultraviolet radiation that causes sunburns.
But the big reason your skin is more likely to burn has to do with all that fresh powder that skiers and snowboarders crave, especially on perfect, blue-sky days. I’m a snow scientist at Colorado State University and an avid skier. There are many ways that snow conditions affect how much your skin will burn.
Fresh snow is very reflective
When you’re out in the snow, a lot of the solar radiation your skin receives is reflected from the snow itself. The amount of radiation reflected is known as albedo.
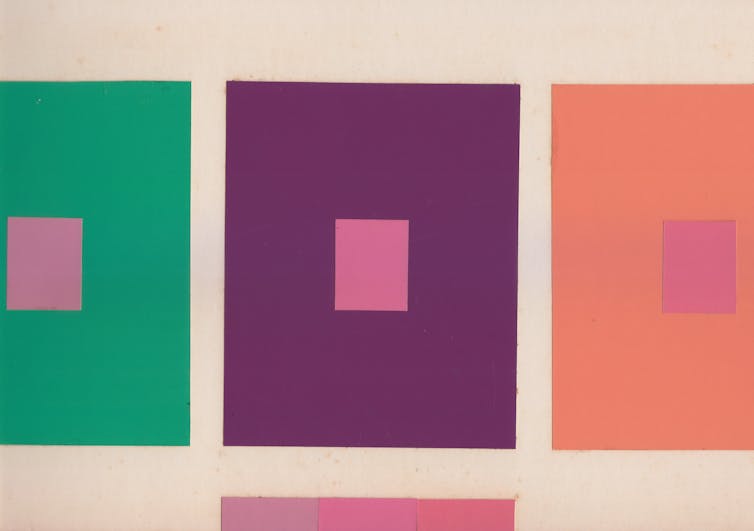
Fresh powder snow can have an albedo of almost 95%, meaning it reflects almost all of the Sun’s radiation that hits it. It’s much more reflective than older snow, which becomes less shiny. Fresh snow has a lot of surfaces to reflect the Sun’s rays. As snow ages, the snow crystal becomes more round and there are fewer surfaces to reflect light.

Steven Fassnacht/Colorado State University, CC BY

Steven Fassnacht/Colorado State University, CC BY
Having lots of fresh snow increases albedo because the Sun penetrates into the powder, reflecting off the small, newly fallen crystals. Think about starting a car after 6 inches of fresh snow fell. Some light still makes its way through the snow-covered windshield.
Having only an inch of powder on crust is not as reflective as knee-deep fresh powder. Shallow snow is less reflective.

A lot of people want to ski on what are known as bluebird days, when there is deep, fresh powder under a clear blue sky following a big snow dump. However, this provides the perfect conditions to burn from two directions: lots of Sun coming down from above and high albedo reflecting it back to your face from below. Clouds block sunlight, with only about one-third of the Sun’s radiation making it through a fully overcast sky.
Which side of the mountain also matters
Where you are on the mountain also makes a difference.
The slope and the direction that the slope faces, called aspect, also influences the intensity of the Sun on a surface. North-facing slopes in the Northern Hemisphere get less direct sunlight in the winter, when the Sun is farther south in the sky, so they stay cooler.

Steven Fassnacht/Colorado State University, CC BY
A lot of the runs at Northern Hemisphere ski resorts face north, so the snow melts slower. The snow also varies from the top of the mountain to the base. There is more snow up high, and the snow melts slower there, so the albedo is higher at the top of the mountain than at the base.
How to reduce the risk of sunburn
To avoid sunburns, skiers and snowboarders need to take all of those characteristics into account.
Because solar radiation is reflecting back up, people out in the snow should put sunscreen on the bottom of their noses, around their ears and on their chins, as well as the usual places.
Most sunscreen also needs to be reapplied every two hours, particularly if you’re likely to sweat it off, wipe it off, or wear it off while playing on the slopes. However, surveys show that few people remember to do this. Wearing clothing with UV protection to cover as much skin as possible can also help.
These methods can help protect your skin from burning and the risks of cancer and premature aging that come with it. Snow lovers need to remember that they face higher sunburn risks on the slopes than they might be accustomed to.![]()
Steven R. Fassnacht, Professor of Snow Hydrology, Colorado State University
This article is republished from The Conversation under a Creative Commons license. Read the original article.