Mississippi Today
‘This is where it starts’: UMMC summit aims to increase number of Black men in health care
Brielan Terrell sat a few rows behind the other boys in the auditorium at the University of Mississippi Medical Center.
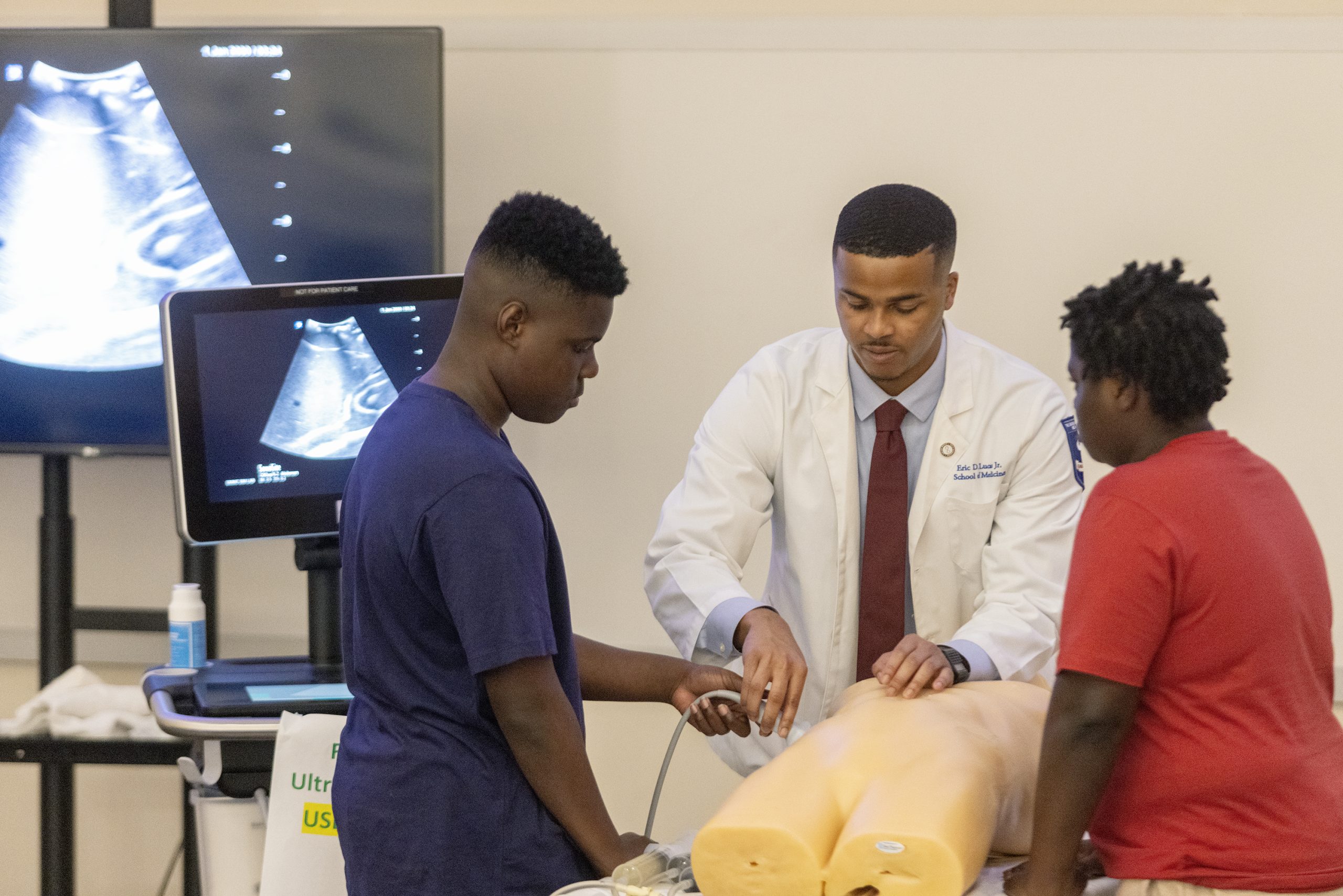
The 18-year-old leaned forward, listening intently, as Eric Lucas Jr., a fourth-year medical student, demonstrated how to perform an ultrasound. As Lucas slid the probe across a medical manikin’s chest, he peppered his audience, about 35 young Black men clad in sports coats and bowties, with questions.
“Can anyone tell me what a stable blood pressure is?” he asked.
Terrell raised his hand and answered correctly: “120 over 80.”
Lucas beamed. This was exactly what he imagined three years ago when he came up with the idea for the Black Men in Health Care Empowerment Summit.
The one-day summer program saw its third cohort on Saturday, as over 100 middle and high school students from all over the state visited UMMC for tours and clinical simulations. Aimed at encouraging young Black men to pursue health care careers, Lucas pitched his idea during his first year at UMMC.
“That’s how I was raised,” he said. “When you walk through the door, you should help someone to walk in.”
Lucas, a graduate of Mississippi State University and native of Ocean Springs, always had a career in health care in his sights.
He remembers getting a microscope kit for a gift when he was 4.
“Science has always kind of been my thing,” Lucas admitted.

Growing up with a dentist for a mom and a critical care intensivist for a dad, Lucas always knew being a physician was a real career option. But he also knows that’s not the case for many Black kids in Mississippi, including some of his medical school classmates.
“One day, we were all hanging out, and I was like, ‘Man, how cool would it have been if we had a summer camp that brought us through all the medical schools and just getting exposed to what it takes?’” Lucas recounted.
“If you don’t see it, you’re not going to believe it.”
And so the summit was born.
In Mississippi, a state with one of the worst health outcomes for people of color in the country, getting more young Black people involved in health care could make all the difference.
That’s why Dr. Demondes Haynes jumped at the opportunity to make Lucas’ dream a reality at UMMC.
“Just to let students know that a career in health care is an option,” he said. “Not that everybody that’s here today will become a doctor or dentist or a nurse, but we want them to know that it is an option.”

Haynes, associate dean for admissions at UMMC, said the only demographic group that had a decrease in students applying and being admitted to medical school in the past 40 years were Black men.
Less than 6% of doctors in the United States identify as Black or African American, though Black people make up about 12% of the population.
Though it’s been shown that, when Black patients are treated by Black doctors, they’re happier with their health care and are more likely to get the preventative care they need, one recent study linked the prevalence of Black doctors to longer life expectancy among Black populations for the first time.
Black men have the shortest life expectancy in the country. The potential power of increasing the number of Black men in the health care field is clear.
“We, as a medical center, want to improve the lives of Mississippians overall,” Haynes said. “This is important because we want to invest in students to contribute to Mississippi. So our hope is that some of these will enter the healthcare field and hopefully stay in Mississippi and improve life in Mississippi for all citizens.”
Throughout the morning, Black medical students and doctors led summit participants — including Terrell — through tours, panels and lectures.
As one of the oldest students in attendance, Terrell lagged behind to talk to medical professionals and raised his hand often. The incoming freshman at the University of Southern Mississippi had a lot on his mind.
During downtime of the ultrasound session, Terrell started chatting with Jaharah Muhammad, a third-year medical student, about his interest in pharmacy.
“Are you going to stay in Mississippi?” she asked.
He answered indecisively.
Later, moments before the students filed out of the auditorium and the next group of medical students and doctors would try to open their eyes to the possibilities of a career in health care, Muhammad shared some parting words.
“Consider staying here,” she said. “If you want more people who look like y’all in health care, this is where it starts.”
This article first appeared on Mississippi Today and is republished here under a Creative Commons license.
Mississippi Today
1964: Mississippi Freedom Democratic Party was formed
April 26, 1964

Civil rights activists started the Mississippi Freedom Democratic Party to challenge the state’s all-white regular delegation to the Democratic National Convention.
The regulars had already adopted this resolution: “We oppose, condemn and deplore the Civil Rights Act of 1964 … We believe in separation of the races in all phases of our society. It is our belief that the separation of the races is necessary for the peace and tranquility of all the people of Mississippi, and the continuing good relationship which has existed over the years.”
In reality, Black Mississippians had been victims of intimidation, harassment and violence for daring to try and vote as well as laws passed to disenfranchise them. As a result, by 1964, only 6% of Black Mississippians were permitted to vote. A year earlier, activists had run a mock election in which thousands of Black Mississippians showed they would vote if given an opportunity.
In August 1964, the Freedom Party decided to challenge the all-white delegation, saying they had been illegally elected in a segregated process and had no intention of supporting President Lyndon B. Johnson in the November election.
The prediction proved true, with white Mississippi Democrats overwhelmingly supporting Republican candidate Barry Goldwater, who opposed the Civil Rights Act. While the activists fell short of replacing the regulars, their courageous stand led to changes in both parties.
This article first appeared on Mississippi Today and is republished here under a Creative Commons Attribution-NoDerivatives 4.0 International License.![]()
Mississippi Today
Mississippi River flooding Vicksburg, expected to crest on Monday
Warren County Emergency Management Director John Elfer said Friday floodwaters from the Mississippi River, which have reached homes in and around Vicksburg, will likely persist until early May. Elfer estimated there areabout 15 to 20 roads underwater in the area.
“We’re about half a foot (on the river gauge) from a major flood,” he said. “But we don’t think it’s going to be like in 2011, so we can kind of manage this.”
The National Weather projects the river to crest at 49.5 feet on Monday, making it the highest peak at the Vicksburg gauge since 2020. Elfer said some residents in north Vicksburg — including at the Ford Subdivision as well as near Chickasaw Road and Hutson Street — are having to take boats to get home, adding that those who live on the unprotected side of the levee are generally prepared for flooding.



“There are a few (inundated homes), but we’ve mitigated a lot of them,” he said. “Some of the structures have been torn down or raised. There are a few people that still live on the wet side of the levee, but they kind of know what to expect. So we’re not too concerned with that.”
The river first reached flood stage in the city — 43 feet — on April 14. State officials closed Highway 465, which connects the Eagle Lake community just north of Vicksburg to Highway 61, last Friday.

Elfer said the areas impacted are mostly residential and he didn’t believe any businesses have been affected, emphasizing that downtown Vicksburg is still safe for visitors. He said Warren County has worked with the U.S. Army Corps of Engineers and the Mississippi Emergency Management Agency to secure pumps and barriers.
“Everybody thus far has been very cooperative,” he said. “We continue to tell people stay out of the flood areas, don’t drive around barricades and don’t drive around road close signs. Not only is it illegal, it’s dangerous.”
NWS projects the river to stay at flood stage in Vicksburg until May 6. The river reached its record crest of 57.1 feet in 2011.




This article first appeared on Mississippi Today and is republished here under a Creative Commons Attribution-NoDerivatives 4.0 International License.![]()
Mississippi Today
With domestic violence law, victims ‘will be a number with a purpose,’ mother says
Joslin Napier. Carlos Collins. Bailey Mae Reed.
They are among Mississippi domestic violence homicide victims whose family members carried their photos as the governor signed a bill that will establish a board to study such deaths and how to prevent them.
Tara Gandy, who lost her daughter Napier in Waynesboro in 2022, said it’s a moment she plans to tell her 5-year-old grandson about when he is old enough. Napier’s presence, in spirit, at the bill signing can be another way for her grandson to feel proud of his mother.
“(The board) will allow for my daughter and those who have already lost their lives to domestic violence … to no longer be just a number,” Gandy said. “They will be a number with a purpose.”
Family members at the April 15 private bill signing included Ashla Hudson, whose son Collins, died last year in Jackson. Grandparents Mary and Charles Reed and brother Colby Kernell attended the event in honor of Bailey Mae Reed, who died in Oxford in 2023.
Joining them were staff and board members from the Mississippi Coalition Against Domestic Violence, the statewide group that supports shelters and advocated for the passage of Senate Bill 2886 to form a Domestic Violence Facility Review Board.
The law will go into effect July 1, and the coalition hopes to partner with elected officials who will make recommendations for members to serve on the board. The coalition wants to see appointees who have frontline experience with domestic violence survivors, said Luis Montgomery, public policy specialist for the coalition.
A spokesperson from Gov. Tate Reeves’ office did not respond to a request for comment Friday.
Establishment of the board would make Mississippi the 45th state to review domestic violence fatalities.
Montgomery has worked on passing a review board bill since December 2023. After an unsuccessful effort in 2024, the coalition worked to build support and educate people about the need for such a board.
In the recent legislative session, there were House and Senate versions of the bill that unanimously passed their respective chambers. Authors of the bills are from both political parties.
The review board is tasked with reviewing a variety of documents to learn about the lead up and circumstances in which people died in domestic violence-related fatalities, near fatalities and suicides – records that can include police records, court documents, medical records and more.
From each review, trends will emerge and that information can be used for the board to make recommendations to lawmakers about how to prevent domestic violence deaths.
“This is coming at a really great time because we can really get proactive,” Montgomery said.
Without a board and data collection, advocates say it is difficult to know how many people have died or been injured in domestic-violence related incidents.
A Mississippi Today analysis found at least 300 people, including victims, abusers and collateral victims, died from domestic violence between 2020 and 2024. That analysis came from reviewing local news stories, the Gun Violence Archive, the National Gun Violence Memorial, law enforcement reports and court documents.
Some recent cases the board could review are the deaths of Collins, Napier and Reed.
In court records, prosecutors wrote that Napier, 24, faced increased violence after ending a relationship with Chance Fabian Jones. She took action, including purchasing a firearm and filing for a protective order against Jones.
Jones’s trial is set for May 12 in Wayne County. His indictment for capital murder came on the first anniversary of her death, according to court records.
Collins, 25, worked as a nurse and was from Yazoo City. His ex-boyfriend Marcus Johnson has been indicted for capital murder and shooting into Collins’ apartment. Family members say Collins had filed several restraining orders against Johnson.
Johnson was denied bond and remains in jail. His trial is scheduled for July 28 in Hinds County.
He was a Jackson police officer for eight months in 2013. Johnson was separated from the department pending disciplinary action leading up to immediate termination, but he resigned before he was fired, Jackson police confirmed to local media.
Reed, 21, was born and raised in Michigan and moved to Water Valley to live with her grandparents and help care for her cousin, according to her obituary.
Kylan Jacques Phillips was charged with first degree murder for beating Reed, according to court records. In February, the court ordered him to undergo a mental evaluation to determine if he is competent to stand trial, according to court documents.
At the bill signing, Gandy said it was bittersweet and an honor to meet the families of other domestic violence homicide victims.
“We were there knowing we are not alone, we can travel this road together and hopefully find ways to prevent and bring more awareness about domestic violence,” she said.
This article first appeared on Mississippi Today and is republished here under a Creative Commons Attribution-NoDerivatives 4.0 International License.
-

 News from the South - Florida News Feed6 days ago
News from the South - Florida News Feed6 days agoJim talks with Rep. Robert Andrade about his investigation into the Hope Florida Foundation
-

 News from the South - Alabama News Feed5 days ago
News from the South - Alabama News Feed5 days agoPrayer Vigil Held for Ronald Dumas Jr., Family Continues to Pray for His Return | April 21, 2025 | N
-

 Mississippi Today5 days ago
Mississippi Today5 days ago‘Trainwreck on the horizon’: The costly pains of Mississippi’s small water and sewer systems
-

 News from the South - Texas News Feed5 days ago
News from the South - Texas News Feed5 days agoMeteorologist Chita Craft is tracking a Severe Thunderstorm Warning that's in effect now
-

 News from the South - Florida News Feed4 days ago
News from the South - Florida News Feed4 days agoTrump touts manufacturing while undercutting state efforts to help factories
-

 News from the South - Virginia News Feed5 days ago
News from the South - Virginia News Feed5 days agoTaking video of military bases using drones could be outlawed | Virginia
-

 News from the South - Texas News Feed7 days ago
News from the South - Texas News Feed7 days agoNo. 3 Texas walks off No. 9 LSU again to capture crucial SEC softball series
-

 News from the South - Florida News Feed4 days ago
News from the South - Florida News Feed4 days agoFederal report due on Lumbee Tribe of North Carolina’s path to recognition as a tribal nation