Mississippi Today
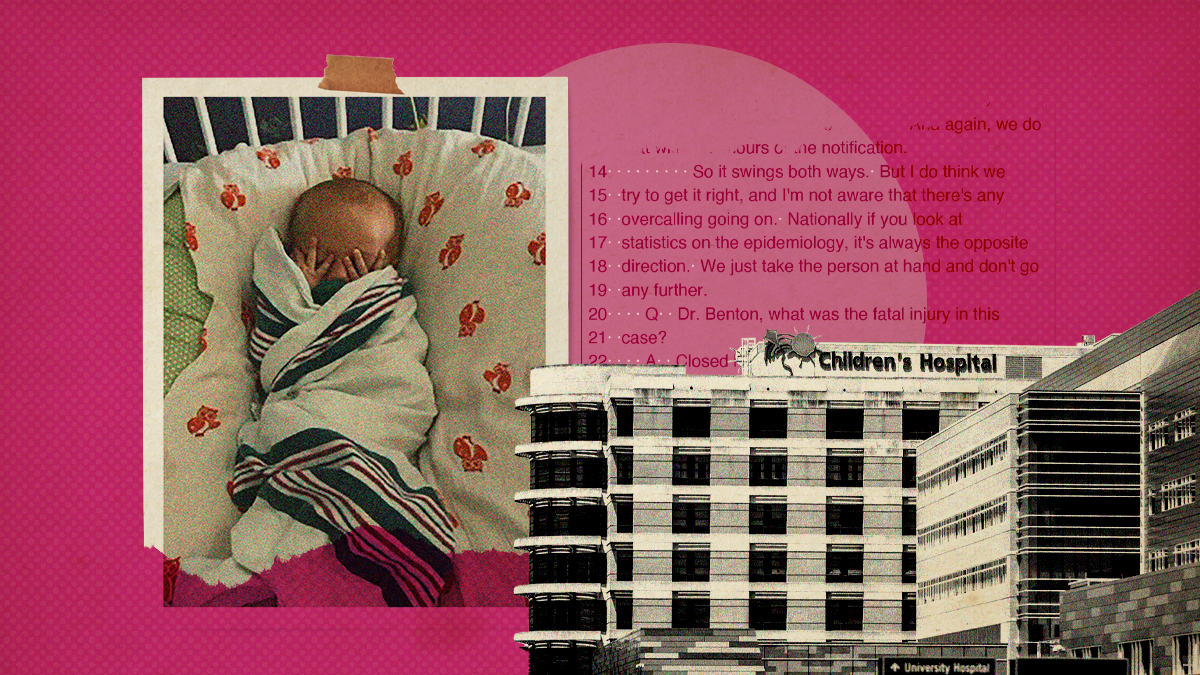
This doctor’s testimony has helped put people in prison. Some say he doesn’t always get it right.
This doctor’s testimony has helped put people in prison. Some say he doesn’t always get it right.
This story is the second part in Mississippi Today’s “Shaky Science, Fractured Families” investigation about the state’s only child abuse pediatrician crossing the line from medicine into law enforcement and how his decisions can tear families apart.Read the full series here.
At Jeffrey Havard’s trial in 2002, medical examiner Dr. Steven Hayne testified the Adams County man had shaken 6-month-old Chloe Britt to death. Her injuries — bleeding in both her brain and retinas — were “consistent with a person violently shaking a small child.”
More than a decade after Havard was convicted and sentenced to death, Hayne changed his mind.
At a hearing in 2017 to determine whether Havard would receive a new trial, Hayne said he believed the science had evolved, and that Chloe could not have died by shaking alone, though he still thought her death was a homicide. The claim that had put Havard on death row — an injury to her rectum meant he had sexually assaulted the baby — disintegrated, as three different experts and Hayne himself now said there was no evidence of sexual abuse.
Havard had long maintained he had been giving Chloe a bath when she slipped from his arms and her head hit the toilet. He put her to bed, and not long after, her mother found her “blue and not breathing.” She died at Natchez Community Hospital on Feb. 21, 2002.
Three defense experts testified in that 2017 hearing that the autopsy findings were consistent with the short fall onto a hard surface Havard had described.
“Chloe died from an impact, a blunt force impact to the head,” said Dr. Michael Baden, former chief medical examiner of New York City and a frequent defense witness in shaken baby syndrome cases. “The shaking of the baby is irrelevant.”
The state called only one witness: Dr. Scott Benton. His testimony helped persuade the judge not to grant Havard a new trial.

Benton was among the first doctors in the country to earn board certification in child abuse pediatrics, a field formally established in 2009. Operating at the intersection of pediatric medicine and forensic pathology, such doctors say they have the tools and expertise to diagnose a crime that specialists in other fields could miss.
Another part of their job is testifying in criminal proceedings involving child abuse. Benton has been a prolific witness, testifying hundreds of times since the mid-1990s. He is the only child abuse pediatrician in Mississippi, one of nine states with just one such specialist.
In an email to Mississippi Today, Benton said the Children’s Safe Center as a group, including him, provides testimony about 12 times a year.
A Mississippi Today investigation found Benton’s testimony has helped keep two Mississippians convicted of shaken baby syndrome behind bars, even though the original expert in each case had changed their conclusions.
Testifying for the prosecution in a Louisiana murder trial, he incorrectly characterized the possible consequences of a rare genetic disorder, claiming it had never been linked to the brain bleeding and swelling that preceded a child’s death, when it had, in multiple peer-reviewed journal articles.
He nearly always testifies against defendants. In one case in which he did testify for the defense, he charged double the hourly rate he has charged Mississippi prosecutors. And his testimony in that case, in which the child survived, struck a different tone from what he gave the prosecution in another shaken baby syndrome case with some similarities, allowing for more uncertainty about the cause of the victim’s injuries.
“I’ve never encountered any system in which a child abuse pediatrician’s work is consistently and meaningfully reviewed,” said Katherine Judson, executive director of the Center for Integrity in Forensic Sciences, a Wisconsin-based nonprofit that advocates for more rigorous and objective scientific evidence in courtrooms. “These folks who testify, it’s very infrequently that I see meaningful review of their work by somebody who’s objective. And honestly the same is true throughout forensic science — we’re always fighting for meaningful review of what analysts are doing.”
Benton declined Mississippi Today’s requests for an interview. He and officials at the University of Mississippi Medical Center also declined to answer a list of questions from Mississippi Today and to respond to a list of reporters’ findings.
“As medical director of the Children’s Safe Center, Dr. Benton has the difficult role of evaluating the evidence in cases of suspected child abuse in any form and rendering a decision based on his training, many years of experience and deep knowledge of the medical literature,” said Dr. Mary Taylor, pediatrics department chair at UMMC, in an emailed statement to Mississippi Today.
“He and his team of trained child abuse specialists provide evidence-supported medical opinions to many governmental agencies that are tasked with ensuring the safety of children. Often times, these children cannot speak for themselves and Dr. Benton’s medical opinions are one part of a defined system of agencies that examine the totality of available evidence about suspected child abuse with the goal of protecting children from exposure to abusive environments.”
A doctor takes on ‘the disingenuous defense people’
Testimony at Havard’s 2017 hearing mirrored a bitter debate within the medical and criminal justice communities. Neurologists, biomechanical engineers, pediatricians and forensic pathologists — along with defense attorneys — have increasingly raised questions about the science behind the decades-accepted diagnosis of shaken baby syndrome.
On the stand, Benton minimized the controversy describing efforts by “the disingenuous defense people” to “attack erroneously the science that supports an abusive event.”
Hayne had claimed at Havard’s 2002 trial that shaking alone had killed Chloe. At the 2017 hearing, Benton said he agreed with Hayne’s more recent determination that Chloe had died of “shaken baby syndrome with impact or blunt force trauma.” When pressed, he acknowledged that he concluded Chloe’s cause of death was “blunt force head trauma”—a possibility never raised in the 2002 trial.
From the late 1980s through the late 2000s, Hayne performed the vast majority of autopsies in Mississippi, usually with a caseload about seven times above national standards. His testimony helped prosecutors win convictions in high profile cases, some of which were later thrown out because his claims were not supported by science. In 2008 the state ended his contract, but there has never been a systematic review of the cases in which his testimony helped lead to convictions.
Havard’s lawyers also asked Benton about an email he sent to investigative reporter Jerry Mitchell, who had written an article raising questions about Havard’s guilt. “As I read the facts put forth in the above sources, I believe they support a homicide,” he wrote in 2012.
On the stand five years later, Benton said he was surprised he had done that.
“I am a careful person,” he said. “First of all, that is not a medical document. I was not offering a medical opinion. I was offering to help, asking for information. Again, I should have waited for more information. Something about the articles that I don’t have or recall what triggered it, but it was the team at the moment that thought, hey, you can help this person, and then whatever I read had some concerns, because it sounded (like the) typical litany in the media attacking Shaken Baby Syndrome as unscientific. Maybe so, maybe not.”
In the end, Adams County Circuit Judge Forrest A. Johnson ordered a new sentencing hearing for Havard, but not a new trial. The new evidence was enough to get him off death row, but he is still serving life without parole.
In Mississippi, at least 11 people have been convicted of shaking a baby to death since 2000.
Those convicted have continued to try to appeal based on new science. In two of those cases, including Havard’s, testimony from Benton has played a key role in preventing people from getting new trials.
Havard’s attorneys told Mississippi Today the case against their client was based on “flawed medicine and junk science” long before Benton got involved, said Jackson-based attorney Graham Carner.
“Fortunately, Dr. Benton recognizes this about the sexual assault allegation — which every single expert who has looked at this case for the state or the defense says is unfounded,” Carner said.
“Dr. Benton’s opinions about SBS, though, are speculative and subjective. They are not the product of a dispassionate scientist but an admitted advocate. Essentially, Dr. Benton’s opinion is that there was child abuse in this case because he says so. That’s not science, and it is dangerous in a courtroom.”
Providing testimony in child abuse trials around the South
According to his curriculum vitae, Benton has provided expert testimony in more than 350 legal proceedings since 1996, from custody disputes to youth court cases to murder trials across Mississippi as well as in Louisiana, Georgia and Alabama.
His testimony creates a funding stream for the Children’s Safe Center at the University of Mississippi Medical Center — one critics including defense attorneys and law professors say can create a sense of alliance with law enforcement and an incentive to side with their interpretation of events.
Records obtained by Mississippi Today show that from July 2015 through February 2022, Benton’s testimony generated more than $140,000 in funding for the center. That’s just a small fraction of the center’s overall budget, which is mostly funded by the state and federal grants.
Resource- and time-strapped public defenders often don’t hire expert witnesses at all, said state public defender André de Gruy. In Mississippi, a judge must approve motions for funding for such witnesses.
The state’s public defense system is a patchwork, with part-time defense lawyers in many counties on fixed-rate contracts representing defendants. In counties without funded public defenders’ offices, they are selected by judges who have an incentive to speed up the process and keep costs down. The more time public defenders spend on a case, the less money they make per hour.
Contract public defenders “either do their own investigation or it doesn’t get done,” de Gruy said. “You look at the prosecution side and they’re all … fully funded offices with support staff and investigators and victim witness coordinators, and they don’t have to worry about whether or not the lights are gonna get cut off because they’re in a county building.”
Although Benton’s value on the stand derives from his expertise in medicine and science, he generally plays for only one team. A UMMC spokesperson said he has testified for the defense “five or six times to his recollection.”
In a deposition in 2017, Benton told Havard’s attorneys he had never testified on behalf of a defendant accused of killing a child. And in every fatal shaken baby syndrome case in which he had testified as of then, he had concluded the syndrome caused the child’s death.
Havard’s case came to his attention because a colleague read a newspaper article that discussed questions about the validity of the conviction. The colleague surmised Benton might be able to contribute to Havard’s defense.
Instead, he wound up testifying for the state. His contract with the Attorney General’s Office stipulated he would be paid $175 an hour to review documents, prepare reports and testify in the case. Records obtained by Mississippi Today show the Children’s Safe Center received $14,251.68 for his work in the case.
The hourly rate of around $175 is somewhat low for a medical doctor, de Gruy said.
“I’ve heard people who’ve gotten experts that said Benton got this wrong,” de Gruy said. “But I’ve never heard that Benton went outside of the established norms of his field or that he fabricated evidence or anything.”
De Gruy pointed to Hayne and Michael West, a dentist whose now-discredited bite mark analysis helped send defendants to death row, as examples of expert witnesses whose work was very wrong for decades and went unchallenged because defendants often couldn’t afford to hire expert witnesses of their own.
Benton’s testimony is different, and de Gruy said he thinks the doctor usually makes the right calls. But in “close calls,” another professional might make a different determination after reviewing the same evidence.
If such cases make it to court, a jury decides who’s right — but they may never hear from an expert witness for the defense.
A rare genetic disorder has been associated with brain bleeding. Dr. Benton said it hasn’t.
Benton has been testifying in cases involving shaken baby syndrome for more than two decades, sometimes providing critical information for the prosecution when there were no eyewitnesses and other evidence was only circumstantial.
On April 3, 1998, 11-month-old Brenda Boudreaux’s mother found her listless in her bed. For the last week, she had been vomiting regularly and suffering from diarrhea but had never been so hard to rouse.
At West Jefferson Medical Center in Marrero, Louisiana, a CT scan found bleeding in her brain. In combination with bleeding retinas, a pediatric ICU doctor determined she was suffering from shaken baby syndrome. A neurosurgeon who operated also found “extremely elevated intracranial pressure,” which he attributed to the syndrome as well.
Benton, who lived in Louisiana at the time, also saw her at the medical center, while she was in a coma. He concluded Brenda had suffered from “Shaken Infant Impact Syndrome and possibly a variant of it called Tin Ear Syndrome.”
After the surgery, she spent a month recovering at a hospital and then went home. But her mother said she was never again the lively and happy baby she had been.
Brenda was hospitalized again in August 1998 and diagnosed with hydrocephalus, an abnormal buildup of fluid in the brain, which doctors also attributed to shaken baby syndrome. A doctor performed surgery to release fluid and bring down the swelling in her brain. He noticed “a tiny hole … leaking a little bit of fluid,” indicating a risk for infection: if fluid could get out, bacteria could get in. Because of that, he inserted a temporary drain that could be replaced with a permanent shunt later.
“That operation went well,” the surgeon, Dr. John Steck, would later say. “That night Brenda had a problem and died.”
Her mother’s boyfriend, Randy Richthofen, had been alone with Brenda for about two hours in the evening before her mother first brought her to the hospital in April. He was charged with second degree murder.
During his trial, the prosecution frequently asked doctors on the stand about a rare genetic condition Brenda had called Adams-Oliver Syndrome. The symptoms vary widely. Shortened limbs and missing pieces of skull and scalp are hallmarks.
One of Brenda’s arms “stopped at the elbow,” as her mother said during the trial. Her other hand was missing three fingers, and she had an artificial eye. Benton also noticed “a little piece of her skin” at the back of her head that had not grown properly from birth.
No geneticist testified. Instead, each doctor — who acknowledged they lacked expertise in the syndrome — said they knew of no relationship between Adams-Oliver and Brenda’s symptoms. Benton went into the greatest detail, explaining how he ruled out Adams-Oliver as a factor in Brenda’s injuries.
“We accessed the large international and national databases … everything ever known about it (the disorder),” he testified. “As best as we can read, of all the children that have been diagnosed with this, and from what we can gather from the medical records of Brenda, the brain and the developmental function is normal, meaning they have normal intelligence and normal brain function.”
The bleeding in Brenda’s brain and the hydrocephalus could not be associated with her genetic condition, Benton said.
But scholarly articles on Adams-Oliver published before 2000, when Benton testified, indicate otherwise.
One 1994 study published in the American Journal of Medical Genetics documented people with the syndrome exhibiting “mental retardation” and hydrocephaly.
“She developed acute hydrocephaly at age 7 days and required a ventriculo-peritoneal shunt,” the authors wrote of one patient. “The infant died at age 3 months during cardiac catheterization.”
A 1993 case report in the Archives of Disease in Childhood documented a child who nearly died from bleeding in the brain associated with scalp and skull defects.
It’s not clear if Benton read the studies, which were published in peer-reviewed medical journals, or if he did not actually review “everything ever known about” Adams-Oliver. What is clear is that his claims directly conflicted with scientific information available at the time.
Instead of considering her genetic disorder, Benton determined she had been shaken.
At Richthofen’s trial, he invoked the triad of symptoms related to shaken baby syndrome diagnosis without using that word.
Richthofen was convicted of second-degree murder and sentenced to life in prison. He remains in prison today.
Doctors’ testimony key to conviction
Matthew James Nolan, a young father in Louisiana’s Sabine Parish, south of Shreveport, quit his job to spend more time with his newborn son, Caleb. On the morning of June 27, 2002, Nolan carried his son into the kitchen to give him a bottle. While preparing the formula and holding Caleb in one arm, Nolan would later say, he dropped the baby, who landed on his buttocks and back on the kitchen floor, and almost immediately stopped breathing.
Nolan was charged with second-degree murder.
The primary evidence against him was the medical experts’ testimony about Caleb’s injuries, which were used to establish the prosecution’s theory of how Caleb had died — shaking, possibly with impact — and who had done it based on the timing: Nolan.
During the bench trial, four doctors testified: Caleb’s regular pediatrician, a critical care doctor who treated him before he died, the coroner, and Benton.
The critical care pediatrician gave her opinion as to what could have caused Caleb’s injuries: “Severe shaking, possibly with what some people call shaken impact syndrome where the baby is shaken but the head’s also hit on something.”
Benton gave a computer presentation on shaken baby syndrome and explained why he, too, didn’t believe Nolan’s explanation. A fall from about four feet would not have caused retinal bleeding and subdural hemorrhage, he said. And such a fall should have caused visible injury to the skin or skull, and there was none.
Instead, Caleb had a “diffuse brain injury” that could only have been caused by acceleration and deceleration forces, like those generated by shaking.
The bleeding was concentrated on the left side of Caleb’s brain. But Benton insisted that didn’t mean there had been an impact there.
Benton dismissed the suggestion that bruising on Caleb’s buttocks could have been caused by a fall like the one Nolan described.
“The diaper is like an airbag,” he said on the stand.
For Betty Maupin, Nolan’s mother and Caleb’s grandmother, that line stands out when she thinks back on her son’s trial.
“Don’t tell me a 3-week-old infant — their little necks are like noodles,” she said. “They tell you to be so careful, support their head. But that’s OK — you can drop them from about 42 inches. if they drop on their diaper, it’ll act as an airbag.”
Nolan’s defense called no medical experts to refute Benton’s testimony.
At 23, Nolan was convicted and sentenced to life in prison without parole. Because he had opted for a bench trial at the advice of his attorney, only one person — the judge — decided the outcome.
“They never said exactly (how or why he would have killed his son) other than they would just bring up — ‘shake and slam. Shake and slam,’” Maupin said. “Dr. Benton has a lot of cases. Shaken and slammed.”
Nolan is still in prison. He was recently transferred from Angola to Elayn Hunt, making Maupin’s drive to see him about an hour longer each way. Her son’s experience showed her the power doctors can wield within the criminal justice system.
“There’s an injury, but if a doctor says it was not accidental, they’ve ruined the family’s life,” she said. “That’s the part that I guess is disturbing the most to me– how a doctor’s opinion can destroy a family.”
Benton’s style as an expert witness has led defense attorneys to raise concerns about his credibility.
In 2015, Trenique Faciane of Lacombe, La., was charged with second-degree murder in the death of 22-month-old Madison Parrott, a foster child in her care. Faciane had no criminal record. She was accused of beating the child with a hair brush, shaking her and dropping her in a bathtub. Faciane said she had been trying to wash ointment off the little girl in the tub when, slippery and sliding around, she hit her head on the faucet. The cause of death was multiple blunt-force trauma with bleeding in the brain.
Attorney James Blazek, representing her pro bono, reached out to Benton in 2016 in hopes he could provide expert testimony during her trial. Blazek said Benton agreed to assist.
But in 2017, Blazek learned the prosecution had hired Benton.
“I’ve never had a case where an expert witness discussed the matter with me and then received material from me and had … what I considered a confidential discussion do that,” he said. “In my opinion, I think it was highly unusual, highly unethical.”
A defense attorney in a Mississippi case in 2018 asked Benton on the stand about Blazek’s accusations. He said he had spoken with Blazek, but denied that he had agreed to consult with him. Benton and UMMC did not respond to Mississippi Today’s questions about the case.
Faciane entered an Alford plea to manslaughter, meaning she did not admit she was guilty but that a guilty verdict would be the likely outcome of a trial because attorneys felt that as a Black woman accused of killing a white child on trial in St. Tammany Parish, she would be unlikely to be acquitted, Blazek said. The sentencing hearing became almost a trial on its own, as Faciane continued to maintain her innocence.
Faciane was sentenced to 30 years in prison, and Benton’s testimony was key.
“Dr. Benton, the expert in pediatric forensic medicine, who is well-known in this area and throughout the Southeast, has examined hundreds if not thousands of injured children, some of whom were abused, some of whom were not abused,” Judge Richard A. Swartz Jr. said in announcing the sentence. “His opinion was based on the medical records, the photographs of the child. And his opinion was that it was trauma, and the trauma to Madison Parrott was not accidental nor self-inflicted.”
Benton’s testimony keeps shaken baby syndrome defendant in prison
Not long after Havard’s 2017 hearing, the state of Mississippi hired Benton to push back on another appeal effort.
Tasha Shelby was convicted of capital murder in 2000 in the death of her fiance’s 2-year-old son Bryan Thompson IV. Prosecutors alleged she had killed the child by shaking his head and banging it against something. She was sentenced to life in prison.
But in the weeks before his death, little Bryan’s eyes had been bloodshot, and relatives noticed he would sometimes stare into space in a way that made his grandmother wonder after his death whether he had been having seizures.
In 2015, the medical examiner who had ruled little Bryan’s death a homicide reexamined medical records and his own files. He concluded a family history of seizures may have played a role in the toddler’s death, and revised the manner of death from homicide to accident.
Shelby sought a new trial based on that revised opinion and on the evolution of the science behind shaken baby syndrome.

During the hearing to decide whether she would receive a new trial, the state again designated a single expert witness: Dr. Scott Benton.
Shelby’s attorneys filed a motion to exclude his testimony.
“His report proffers opinions on cause and manner of death and biomechanics, notwithstanding his lack of experience or training in forensic pathology and biomechanics,” the memo claimed.
The memo also pointed out the report Benton provided to the state included a chart organized around questions that had nothing to do with medicine. Looking at pieces of evidence, he asked “New since trial?” and “Would produce a different result or verdict?”
“The inclusion of this chart demonstrates that Dr. Benton interprets his role here not as an objective expert offering a medical opinion to the court, but as a member of the State’s legal team itself, skewing his opinion to specifically support the State’s theory,” Shelby’s attorneys wrote. “His bias taints his conclusions, and renders his report unreliable.”
The court denied the motion, finding Benton was qualified in child abuse pediatrics and pediatric forensic medicine.
During Shelby’s hearing, Benton testified he believed neither seizures nor a short fall played a role in little Bryan’s death. He said the injuries had to have happened within a tight time frame, hours before the boy was declared dead.
Though there were indications of external impact, Benton said there also had to be “an element of acceleration/deceleration” — of shaking.
Here, too, he minimized the idea that “shaken baby syndrome” is a controversial diagnosis.
“There certainly have been challenges to the concept and there certainly has been some evolution as (to) our understanding it,” Benton said. “But as we sit here today, the majority of physicians that are involved in these types of determinations have accepted that shaking, certainly shaking with impact, is injurious to a child. Additionally, shaking alone is considered to be injurious to a child.”
Shelby’s defense presented four expert witnesses, including the medical examiner who had originally testified for the state a decade and a half earlier.
A Harrison County Circuit Court judge declined to grant Shelby’s appeal. In upholding that decision, the Court of Appeals cited Benton’s testimony as determinative: his willingness to say what had been said at her first trial effectively negated the new perspectives her attorneys presented.
The hearing was “a battle of experts,” the court wrote. “Dr. Benton was a qualified expert witness, and he responded to each of the points raised by Shelby’s experts.”
A different view of doubt when testifying for the prosecution
In 2022, when Benton was an expert witness for the defense in an Alabama head trauma case, his testimony took a different approach in evaluating the possible explanations for the victim’s injuries.
Two-month-old Kian Mixon came to the hospital with a brain bleed, retinal hemorrhages, a busted lip and bruises or discoloration behind his ears, according to court documents. His father, Michael Mixon, was charged with aggravated child abuse.
This time, Benton listed the range of explanations for subdural hematoma.
“There’s a long list of things that can cause subdural hematomas, the most common of which is trauma,” he said.
He rattled off the other explanations: metabolic disorders, bleeding disorders, brain abnormalities, collagen vascular diseases. He had also considered and ruled out these explanations in his written report on Shelby. But on the stand in her case, he emphasized that subdural hematoma was most commonly caused by “tearing of the bridging vessels,” which run between the skull and the brain’s surface.
“To get the tearing of those vessels, you need to have that acceleration/deceleration,” he said.
In the Mixon case, he said it was impossible to know whether the child had experienced seizures because the hospital had apparently not performed the proper testing.
“Many of the head injuries, particularly with involving the bleeds that we see here, have what’s called non-convulsive seizures,” Benton said. “So we already suspect the child may have had a seizure by what the father reported. That has the sounds of a seizure and the recovery from a seizure. You can’t just look at an infant or all infants and know that they’re seizing. You have to put an EEG on them.”
Yet when he evaluated little Bryan’s injuries and the history given by his family — describing spells of staring into space and other behaviors they believed indicated seizures — Benton minimized that information as evidence that the child had had seizures, even though no EEG had been performed.
He also said a seizure would not have caused little Bryan’s injuries.
“The literature is clear that the most common cause of subdural hematoma and subarachnoid hemorrhages in this age group is trauma whether accidental or inflicted,” he wrote in his report on Shelby. “It is usually from severe acceleration/deceleration force; i.e. whiplash motion with or without impact.”
In Mixon’s case, Benton argued that medicine could not use the evidence to precisely date the child’s brain bleed, meaning the defendant couldn’t be identified simply because he had most recently been with the child.
Testifying against Shelby, he concluded that little Bryan’s injuries had been sustained after 9 p.m. the night before he died, based in part on the autopsy findings of the child’s brain, which implicated Shelby.
When you bleed, Benton said then, the body quickly breaks down the red blood cells and sends in inflammatory cells. Within a few hours, the bleed looks different.
“There were intact red cells with no organization, which means that blood is fresh and that the body hasn’t yet had time to respond to it,” he said.
Testifying on behalf of Mixon just a few years later, he said “blood can look fresh on a CT for up to two weeks. So you can’t look at it and say that it happened in a specific time interval. That’s not possible.”
He was comparing two different types of evidence: autopsy records and CT scans. Yet his testimony in the Mixon case allowed for the possibility that a brain injury could be undetected for days or weeks.
There’s also evidence to suggest that red blood cells in subdural hematoma can look intact at autopsy for much longer than the several hours Benton cited in Shelby. A 2019 study published in the peer-reviewed International Journal of Legal Studies looked at infants up to 3 years old who were diagnosed with subdural hematoma during autopsies after their deaths. The study found that red blood cells looked intact or nearly so for 24 hours after the child’s injury. “Distinct” disintegration of the red blood cells was generally seen only after 48 hours.
“That’s just a key part of their case. In this, it’s Tasha because she is alone with the child for this particular period of time,” Valena Beety, an attorney for Shelby, told Mississippi Today. “But if you back it up six hours, she’s not alone. If you back it up 12 hours, she’s not alone.”
In the Mixon case, Benton made twice as much per hour as he charged the state of Mississippi when he testified against Jeffrey Havard: $350 an hour.
Mixon was found not guilty.
“The win could not be possible without the testimony of Dr. Scott Benton from the University of Mississippi,” Mixon’s attorneys wrote on Facebook. “His expert opinions in pediatrics and forensic medicine educated the jury as to the timing of the alleged injuries. Multiple jurors said that was the deciding factor for their verdict.”
After the state Supreme Court ruled against Shelby, her legal team filed a federal appeal. In early February, a federal magistrate judge found that she should have filed her federal appeal for post-conviction relief earlier, before Hurricane Katrina destroyed most of the documents in her case and set off what Beety calls the “goose chase” to obtain medical records.
The judge also said her claims about the unreliability of the science around shaken baby syndrome were not sufficient proof of innocence. Other courts have viewed the controversy as “a battle of the experts,” and that’s what happened here, the judge wrote.
“Shelby presented experts that concluded SBS was no longer a sound diagnosis; while the state presented an expert that testified there was a ‘general acceptance,’ of the diagnosis,” the judge wrote, referring to Benton.
Shelby’s legal team is appealing the decision.
Mississippi Today health editor Kate Royals contributed to this report.
FREE ONLINE JOURNALISM LIKE OURS HAS NEVER MATTERED MORE.
As a nonprofit newsroom, we rely on donations from readers to power our work. Will you invest in the future of independent journalism in Mississippi?
This article first appeared on Mississippi Today and is republished here under a Creative Commons license.
Mississippi Today
Mississippi prepares for another execution
The Mississippi Supreme Court has set the execution of a man who kidnapped and murdered a 20-year-old community college student in north Mississippi 30 years ago.
Charles Ray Crawford, 59, is set to be executed Oct. 15 at the Mississippi State Penitentiary at Parchman, after multiple requests by the attorney general’s office.
Eight justices joined the majority opinion to set the execution, concluding that Crawford has exhausted all state and federal legal remedies. Mississippi Supreme Court Justice T. Kenneth Griffis Jr. wrote the Friday opinion. Justice David Sullivan did not participate.
However, Kristy Noble with the Mississippi Office of Capital Post-Conviction Counsel released a statement saying it will file another appeal with the U.S. Supreme Court.
“”Mr. Crawford’s inexperienced trial counsel conceded his guilt to the jury — against Mr.
Crawford’s timely and repeated objections,” Noble said in the statement. “Mr. Crawford told his counsel to pursue a not guilty verdict. Counsel did just the opposite, which is precisely what the U.S. Supreme Court says counsel cannot do,” Noble said in the statement.
“A trial like Mr. Crawford’s – one where counsel concedes guilt over his client’s express wishes – is essentially no trial at all.”
Last fall, Crawford’s attorneys asked the court not to set an execution date because he hadn’t exhausted appeal efforts in federal court to challenge a rape conviction that is not tied to his death sentence. In June, the U.S. Supreme Court declined to take up Crawford’s case.
A similar delay occurred a decade ago, when the AG’s office asked the court to reset Crawford’s execution date, but that was denied because efforts to appeal his unrelated rape conviction were still pending.
After each unsuccessful filing, the attorney general’s office asked the Mississippi Supreme Court to set Crawford’s execution date.
On Friday, the court also denied Crawford’s third petition for post-conviction relief and a request for oral argument. It accepted the state’s motion to dismiss the petition. Seven justices concurred and Justice Leslie King concurred in result only. Again, Justice Sullivan did not participate.
Crawford was convicted and sentenced to death in Lafayette County for the 1993 rape and murder of North Mississippi Community College student Kristy Ray.
Days before he was set to go to trial on separate aggravated assault and rape charges, he kidnapped Ray from her parents’ Tippah County home, leaving ransom notes. Crawford took Ray to an abandoned barn where he stabbed her, and his DNA was found on her, indicating he sexually assaulted her, according to court records.
Crawford told police he had blackouts and only remembered parts of the crime, but not killing Ray. Later he admitted “he must of killed her” and led police to Ray’s body, according to court records.
At his 1994 trial he presented an insanity defense, including that he suffered from psychogenic amnesia – periods of time lapse without memory. Medical experts who provided rebuttal testimony said Crawford didn’t have psychogenic amnesia and didn’t show evidence of bipolar illness.
The last person executed in Mississippi was Richard Jordan in June, previously the state’s oldest and longest serving person on death row.
There are 36 people on death row, according to records from the Mississippi Department of Corrections.
Update 9/15/25: This story has been updated to include a response from the Mississippi Office of Capital Post-Conviction Counsel
This article first appeared on Mississippi Today and is republished here under a Creative Commons Attribution-NoDerivatives 4.0 International License.
The post Mississippi prepares for another execution appeared first on mississippitoday.org
Note: The following A.I. based commentary is not part of the original article, reproduced above, but is offered in the hopes that it will promote greater media literacy and critical thinking, by making any potential bias more visible to the reader –Staff Editor.
Political Bias Rating: Centrist
The article presents a factual and balanced account of the legal proceedings surrounding a scheduled execution in Mississippi. It includes perspectives from both the state’s attorney general’s office and the defense counsel, without using emotionally charged language or advocating for a particular political stance. The focus on legal details and court decisions reflects a neutral, informative approach typical of centrist reporting.
Mississippi Today
Presidents are taking longer to declare major natural disasters. For some, the wait is agonizing
TYLERTOWN — As an ominous storm approached Buddy Anthony’s one-story brick home, he took shelter in his new Ford F-250 pickup parked under a nearby carport.
Seconds later, a tornado tore apart Anthony’s home and damaged the truck while lifting it partly in the air. Anthony emerged unhurt. But he had to replace his vehicle with a used truck that became his home while waiting for President Donald Trump to issue a major disaster declaration so that federal money would be freed for individuals reeling from loss. That took weeks.
“You wake up in the truck and look out the windshield and see nothing. That’s hard. That’s hard to swallow,” Anthony said.
Disaster survivors are having to wait longer to get aid from the federal government, according to a new Associated Press analysis of decades of data. On average, it took less than two weeks for a governor’s request for a presidential disaster declaration to be granted in the 1990s and early 2000s. That rose to about three weeks during the past decade under presidents from both major parties. It’s taking more than a month, on average, during Trump’s current term, the AP found.
The delays mean individuals must wait to receive federal aid for daily living expenses, temporary lodging and home repairs. Delays in disaster declarations also can hamper recovery efforts by local officials uncertain whether they will receive federal reimbursement for cleaning up debris and rebuilding infrastructure. The AP collaborated with Mississippi Today and Mississippi Free Press on the effects of these delays for this report.
“The message that I get in the delay, particularly for the individual assistance, is that the federal government has turned its back on its own people,” said Bob Griffin, dean of the College of Emergency Preparedness, Homeland Security and Cybersecurity at the University at Albany in New York. “It’s a fundamental shift in the position of this country.”
The wait for disaster aid has grown as Trump remakes government
The Federal Emergency Management Agency often consults immediately with communities to coordinate their initial disaster response. But direct payments to individuals, nonprofits and local governments must wait for a major disaster declaration from the president, who first must receive a request from a state, territory or tribe. Major disaster declarations are intended only for the most damaging events that are beyond the resources of states and local governments.
Trump has approved more than two dozen major disaster declarations since taking office in January, with an average wait of almost 34 days after a request. That ranged from a one-day turnaround after July’s deadly flash flooding in Texas to a 67-day wait after a request for aid because of a Michigan ice storm. The average wait is up from a 24-day delay during his first term and is nearly four times as long as the average for former Republican President George H.W. Bush, whose term from 1989-1993 coincided with the implementation of a new federal law setting parameters for disaster determinations.
The delays have grown over time, regardless of the party in power. Former Democratic President Joe Biden, in his last year in office, averaged 26 days to declare major disasters — longer than any year under former Democratic President Barack Obama.

FEMA did not respond to the AP’s questions about what factors are contributing to the trend.
Others familiar with FEMA noted that its process for assessing and documenting natural disasters has become more complex over time. Disasters have also become more frequent and intense because of climate change, which is mostly caused by the burning of fuels such as gas, coal and oil.
The wait for disaster declarations has spiked as Trump’s administration undertakes an ambitious makeover of the federal government that has shed thousands of workers and reexamined the role of FEMA. A recently published letter from current and former FEMA employees warned the cuts could become debilitating if faced with a large-enough disaster. The letter also lamented that the Trump administration has stopped maintaining or removed long-term planning tools focused on extreme weather and disasters.
Shortly after taking office, Trump floated the idea of “getting rid” of FEMA, asserting: “It’s very bureaucratic, and it’s very slow.”
FEMA’s acting chief suggested more recently that states should shoulder more responsibility for disaster recovery, though FEMA thus far has continued to cover three-fourths of the costs of public assistance to local governments, as required under federal law. FEMA pays the full cost of its individual assistance.
Former FEMA Administrator Pete Gaynor, who served during Trump’s first term, said the delay in issuing major disaster declarations likely is related to a renewed focus on making sure the federal government isn’t paying for things state and local governments could handle.
“I think they’re probably giving those requests more scrutiny,” Gaynor said. “And I think it’s probably the right thing to do, because I think the (disaster) declaration process has become the ‘easy button’ for states.”
The Associated Press on Monday received a statement from White House spokeswoman Abigail Jackson in response to a question about why it is taking longer to issue major natural disaster declarations:
“President Trump provides a more thorough review of disaster declaration requests than any Administration has before him. Gone are the days of rubber stamping FEMA recommendations – that’s not a bug, that’s a feature. Under prior Administrations, FEMA’s outsized role created a bloated bureaucracy that disincentivized state investment in their own resilience. President Trump is committed to right-sizing the Federal government while empowering state and local governments by enabling them to better understand, plan for, and ultimately address the needs of their citizens. The Trump Administration has expeditiously provided assistance to disasters while ensuring taxpayer dollars are spent wisely to supplement state actions, not replace them.”

In Mississippi, frustration festered during wait for aid
The tornado that struck Anthony’s home in rural Tylertown on March 15 packed winds up to 140 mph. It was part of a powerful system that wrecked homes, businesses and lives across multiple states.
Mississippi’s governor requested a federal disaster declaration on April 1. Trump granted that request 50 days later, on May 21, while approving aid for both individuals and public entities.
On that same day, Trump also approved eight other major disaster declarations for storms, floods or fires in seven other states. In most cases, more than a month had passed since the request and about two months since the date of those disasters.
If a presidential declaration and federal money had come sooner, Anthony said he wouldn’t have needed to spend weeks sleeping in a truck before he could afford to rent the trailer where he is now living. His house was uninsured, Anthony said, and FEMA eventually gave him $30,000.
In nearby Jayess in Lawrence County, Dana Grimes had insurance but not enough to cover the full value of her damaged home. After the eventual federal declaration, Grimes said FEMA provided about $750 for emergency expenses, but she is now waiting for the agency to determine whether she can receive more.

“We couldn’t figure out why the president took so long to help people in this country,” Grimes said. “I just want to tie up strings and move on. But FEMA — I’m still fooling with FEMA.”
Jonathan Young said he gave up on applying for FEMA aid after the Tylertown tornado killed his 7-year-old son and destroyed their home. The process seemed too difficult, and federal officials wanted paperwork he didn’t have, Young said. He made ends meet by working for those cleaning up from the storm.
“It’s a therapy for me,” Young said, “to pick up the debris that took my son away from me.”
Historically, presidential disaster declarations containing individual assistance have been approved more quickly than those providing assistance only to public entities, according to the AP’s analysis. That remains the case under Trump, though declarations for both types are taking longer.
About half the major disaster declarations approved by Trump this year have included individual assistance.
Some people whose homes are damaged turn to shelters hosted by churches or local nonprofit organizations in the initial chaotic days after a disaster. Others stay with friends or family or go to a hotel, if they can afford it.
But some insist on staying in damaged homes, even if they are unsafe, said Chris Smith, who administered FEMA’s individual assistance division under three presidents from 2015-2022. If homes aren’t repaired properly, mold can grow, compounding the recovery challenges.

That’s why it’s critical for FEMA’s individual assistance to get approved quickly — ideally, within two weeks of a disaster, said Smith, who’s now a disaster consultant for governments and companies.
“You want to keep the people where they are living. You want to ensure those communities are going to continue to be viable and recover,” Smith said. “And the earlier that individual assistance can be delivered … the earlier recovery can start.”
In the periods waiting for declarations, the pressure falls on local officials and volunteers to care for victims and distribute supplies.
In Walthall County, where Tylertown is, insurance agent Les Lampton remembered watching the weather news as the first tornado missed his house by just an eighth of a mile. Lampton, who moonlights as a volunteer firefighter, navigated the collapsed trees in his yard and jumped into action. About 45 minutes later, the second tornado hit just a mile away.
“It was just chaos from there on out,” Lampton said.
Walthall County, with a population of about 14,000, hasn’t had a working tornado siren in about 30 years, Lampton said. He added there isn’t a public safe room in the area, although a lot of residents have ones in their home.
Rural areas with limited resources are hit hard by delays in receiving funds through FEMA’s public assistance program, which, unlike individual assistance, only reimburses local entities after their bills are paid. Long waits can stoke uncertainty and lead cost-conscious local officials to pause or scale-back their recovery efforts.

In Walthall County, officials initially spent about $700,000 cleaning up debris, then suspended the cleanup for more than a month because they couldn’t afford to spend more without assurance they would receive federal reimbursement, said county emergency manager Royce McKee. Meanwhile, rubble from splintered trees and shattered homes remained piled along the roadside, creating unsafe obstacles for motorists and habitat for snakes and rodents.
When it received the federal declaration, Walthall County took out a multimillion-dollar loan to pay contractors to resume the cleanup.
“We’re going to pay interest and pay that money back until FEMA pays us,” said Byran Martin, an elected county supervisor. “We’re hopeful that we’ll get some money by the first of the year, but people are telling us that it could be [longer].”
Lampton, who took after his father when he joined the volunteer firefighters 40 years ago, lauded the support of outside groups such as Cajun Navy, Eight Days of Hope, Samaritan’s Purse and others. That’s not to mention the neighbors who brought their own skid steers and power saws to help clear trees and other debris, he added.
“That’s the only thing that got us through this storm, neighbors helping neighbors,” Lampton said. “If we waited on the government, we were going to be in bad shape.”
Lieb reported from Jefferson City, Missouri, and Wildeman from Hartford, Connecticut.
Update 98/25: This story has been updated to include a White House statement released after publication.
This article first appeared on Mississippi Today and is republished here under a Creative Commons Attribution-NoDerivatives 4.0 International License.
The post Presidents are taking longer to declare major natural disasters. For some, the wait is agonizing appeared first on mississippitoday.org
Note: The following A.I. based commentary is not part of the original article, reproduced above, but is offered in the hopes that it will promote greater media literacy and critical thinking, by making any potential bias more visible to the reader –Staff Editor.
Political Bias Rating: Center-Left
This article presents a critical view of the Trump administration’s handling of disaster declarations, highlighting delays and their negative impacts on affected individuals and communities. It emphasizes concerns about government downsizing and reduced federal support, themes often associated with center-left perspectives that favor robust government intervention and social safety nets. However, it also includes statements from Trump administration officials defending their approach, providing some balance. Overall, the tone and framing lean slightly left of center without being overtly partisan.
Mississippi Today
Northeast Mississippi speaker and worm farmer played key role in Coast recovery after Hurricane Katrina
The 20th anniversary of Hurricane Katrina slamming the Mississippi Gulf Coast has come and gone, rightfully garnering considerable media attention.
But still undercovered in the 20th anniversary saga of the storm that made landfall on Aug. 29, 2005, and caused unprecedented destruction is the role that a worm farmer from northeast Mississippi played in helping to revitalize the Coast.
House Speaker Billy McCoy, who died in 2019, was a worm farmer from the Prentiss, not Alcorn County, side of Rienzi — about as far away from the Gulf Coast as one could be in Mississippi.
McCoy grew other crops, but a staple of his operations was worm farming.
Early after the storm, the House speaker made a point of touring the Coast and visiting as many of the House members who lived on the Coast as he could to check on them.
But it was his action in the forum he loved the most — the Mississippi House — that is credited with being key to the Coast’s recovery.
Gov. Haley Barbour had called a special session about a month after the storm to take up multiple issues related to Katrina and the Gulf Coast’s survival and revitalization. The issue that received the most attention was Barbour’s proposal to remove the requirement that the casinos on the Coast be floating in the Mississippi Sound.
Katrina wreaked havoc on the floating casinos, and many operators said they would not rebuild if their casinos had to be in the Gulf waters. That was a crucial issue since the casinos were a major economic engine on the Coast, employing an estimated 30,000 in direct and indirect jobs.
It is difficult to fathom now the controversy surrounding Barbour’s proposal to allow the casinos to locate on land next to the water. Mississippi’s casino industry that was birthed with the early 1990s legislation was still new and controversial.
Various religious groups and others had continued to fight and oppose the casino industry and had made opposition to the expansion of gambling a priority.
Opposition to casinos and expansion of casinos was believed to be especially strong in rural areas, like those found in McCoy’s beloved northeast Mississippi. It was many of those rural areas that were the homes to rural white Democrats — now all but extinct in the Legislature but at the time still a force in the House.
So, voting in favor of casino expansion had the potential of being costly for what was McCoy’s base of power: the rural white Democrats.
Couple that with the fact that the Democratic-controlled House had been at odds with the Republican Barbour on multiple issues ranging from education funding to health care since Barbour was inaugurated in January 2004.
Barbour set records for the number of special sessions called by the governor. Those special sessions often were called to try to force the Democratic-controlled House to pass legislation it killed during the regular session.
The September 2005 special session was Barbour’s fifth of the year. For context, current Gov. Tate Reeves has called four in his nearly six years as governor.
There was little reason to expect McCoy to do Barbour’s bidding and lead the effort in the Legislature to pass his most controversial proposal: expanding casino gambling.
But when Barbour ally Lt. Gov. Amy Tuck, who presided over the Senate, refused to take up the controversial bill, Barbour was forced to turn to McCoy.
The former governor wrote about the circumstances in an essay he penned on the 20th anniversary of Hurricane Katrina for Mississippi Today Ideas.
“The Senate leadership, all Republicans, did not want to go first in passing the onshore casino law,” Barbour wrote. “So, I had to ask Speaker McCoy to allow it to come to the House floor and pass. He realized he should put the Coast and the state’s interests first. He did so, and the bill passed 61-53, with McCoy voting no.
“I will always admire Speaker McCoy, often my nemesis, for his integrity in putting the state first.”
Incidentally, former Rep. Bill Miles of Fulton, also in northeast Mississippi, was tasked by McCoy with counting, not whipping votes, to see if there was enough support in the House to pass the proposal. Not soon before the key vote, Miles said years later, he went to McCoy and told him there were more than enough votes to pass the legislation so he was voting no and broached the idea of the speaker also voting no.
It is likely that McCoy would have voted for the bill if his vote was needed.
Despite his no vote, the Biloxi Sun Herald newspaper ran a large photo of McCoy and hailed the Rienzi worm farmer as a hero for the Mississippi Gulf Coast.
This article first appeared on Mississippi Today and is republished here under a Creative Commons Attribution-NoDerivatives 4.0 International License.
The post Northeast Mississippi speaker and worm farmer played key role in Coast recovery after Hurricane Katrina appeared first on mississippitoday.org
Note: The following A.I. based commentary is not part of the original article, reproduced above, but is offered in the hopes that it will promote greater media literacy and critical thinking, by making any potential bias more visible to the reader –Staff Editor.
Political Bias Rating: Centrist
The article presents a factual and balanced account of the political dynamics surrounding Hurricane Katrina recovery efforts in Mississippi, focusing on bipartisan cooperation between Democratic and Republican leaders. It highlights the complexities of legislative decisions without overtly favoring one party or ideology, reflecting a neutral and informative tone typical of centrist reporting.
-
News from the South - North Carolina News Feed6 days ago
What we know about Charlie Kirk shooting suspect, how he was caught
-
Local News7 days ago
Russian drone incursion in Poland prompts NATO leaders to take stock of bigger threats
-
Local News Video7 days ago
Introducing our WXXV Student Athlete of the Week, St. Patrick’s Parker Talley!
-
News from the South - North Carolina News Feed6 days ago
Federal hate crime charge sought in Charlotte stabbing | North Carolina
-
The Center Square7 days ago
Weapon recovered as manhunt continues in Kirk assassination investigation | National
-
News from the South - Tennessee News Feed7 days ago
Middle Tennessee State University dean filed over Kirk comments | Tennessee
-
News from the South - Arkansas News Feed6 days ago
NW Arkansas Championship expected to bring money to Rogers
-
Our Mississippi Home5 days ago
Screech Owls – Small but Cute