Mississippi Today
See running total of how much money Mississippi is turning down by not expanding Medicaid
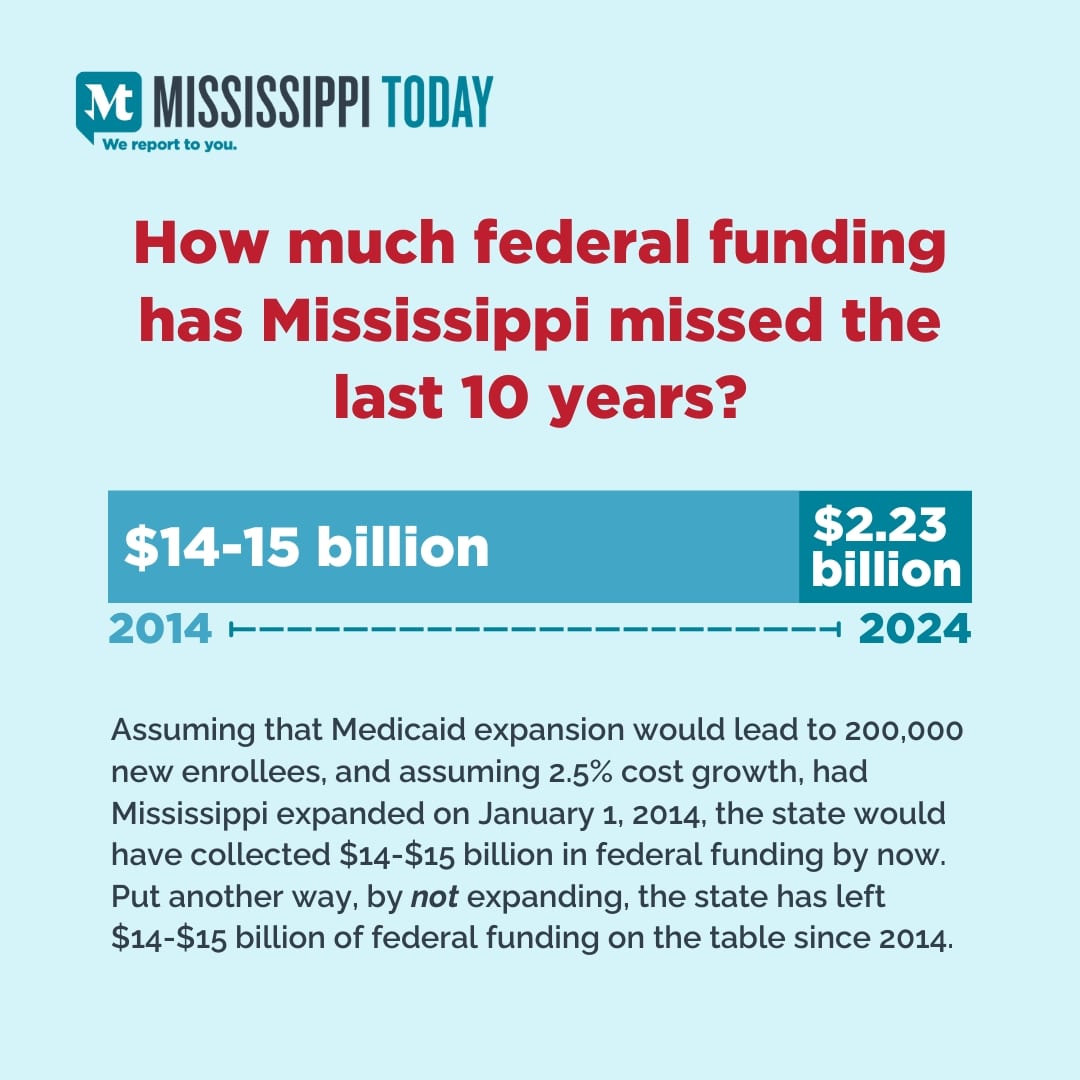
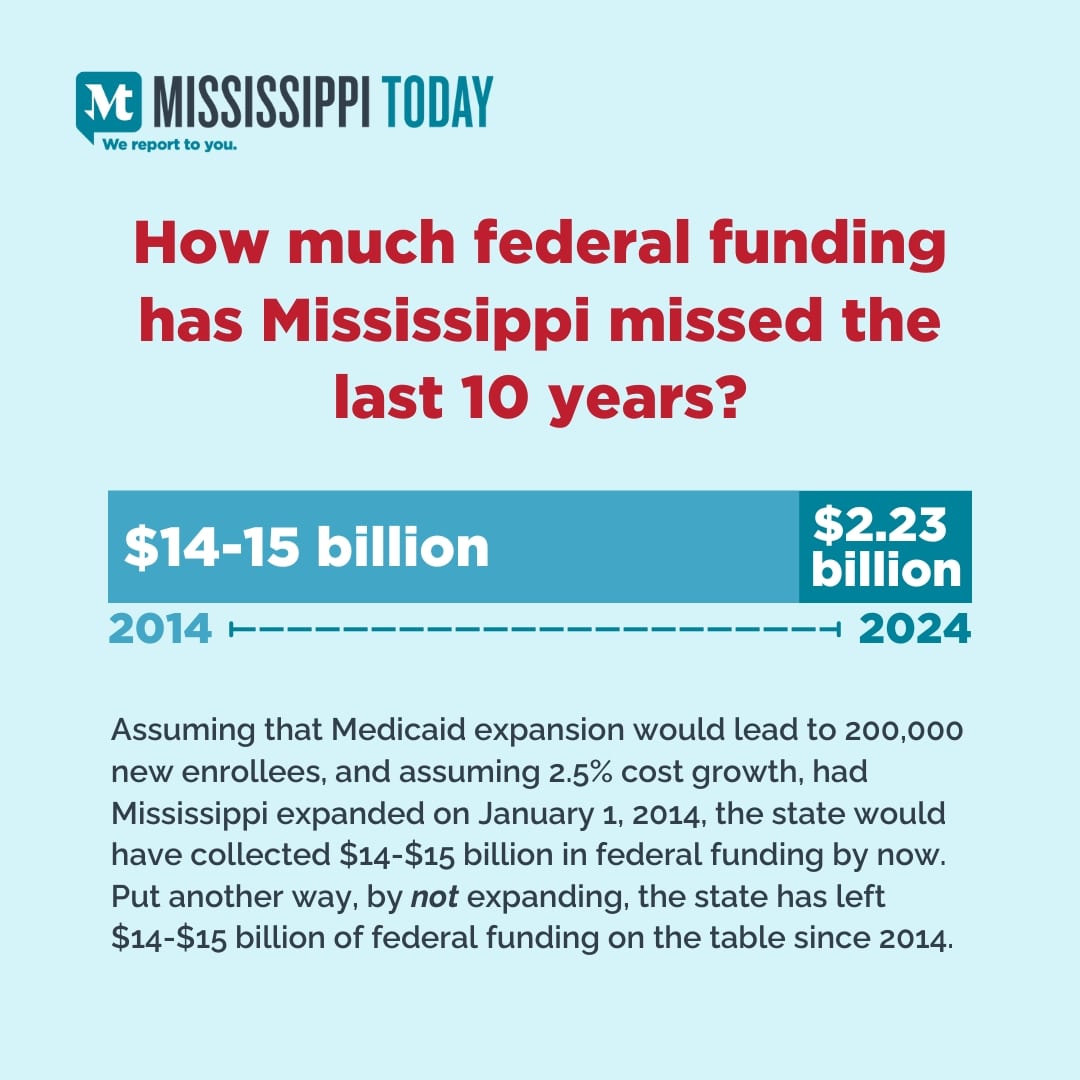
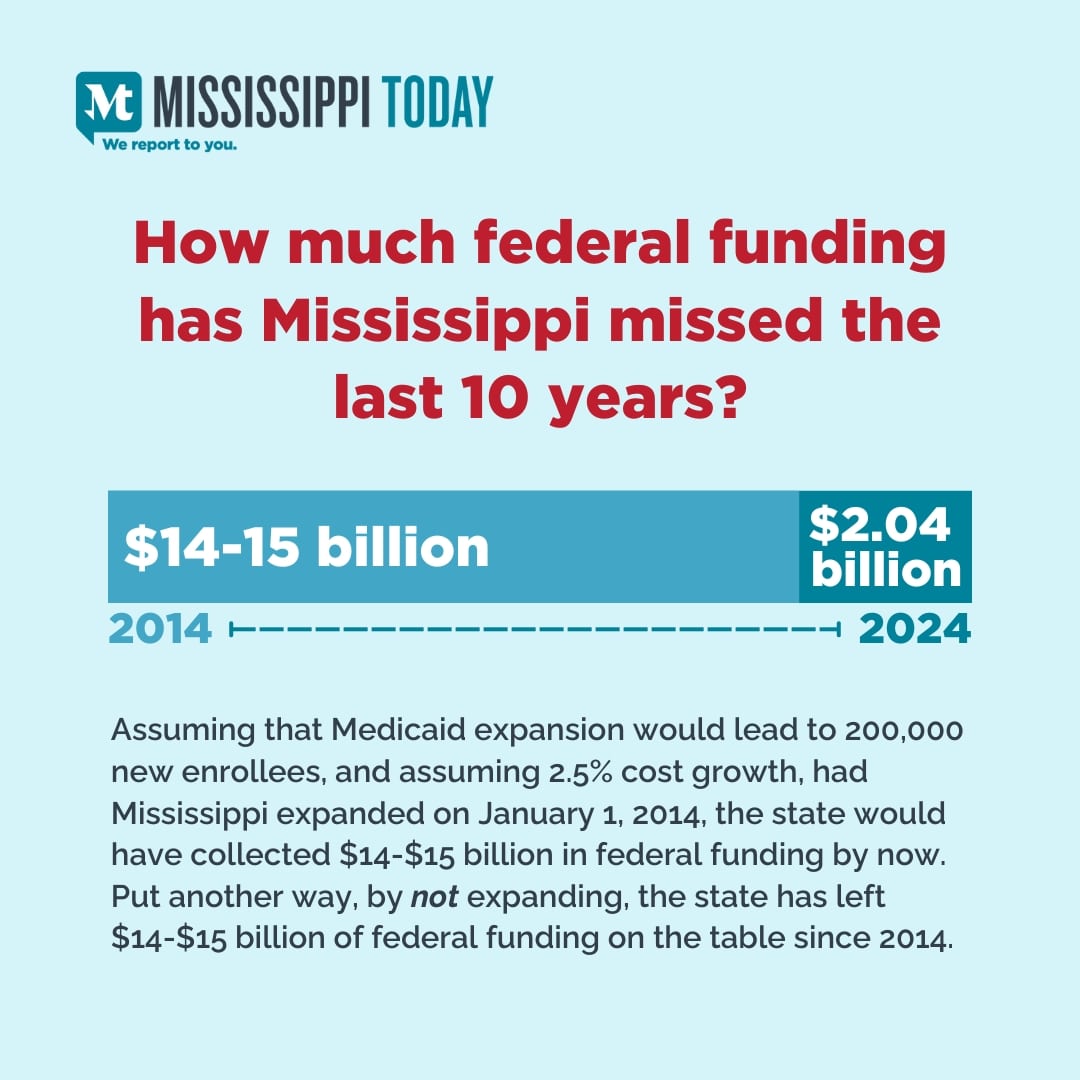
Mississippi would receive an additional $2.04 billion the first year Medicaid was expanded to provide health care coverage for the working poor, according to projections compiled in June by the state’s University Research Center.
Based on that projection, Mississippi Today is unveiling a digital tracker that will run continuously displaying how much money the state is losing in federal funds by not expanding Medicaid. The tracker reflects the amount of money loss per millisecond for the year based on Medicaid expansion beginning on the start of the fiscal year, July 1st.
How much federal funding has Mississippi turned down this year?
The tracker is not exact: The amount of Medicaid money the state receives is based on a number of factors, primarily the health care needs of those covered by Medicaid. Medicaid provides funds to health care providers for rendering medical services to those who qualify for Medicaid.
The state might receive more federal Medicaid funds, for example, during a flu or COVID-19 outbreak because Medicaid recipients would be receiving more health care.
But for the sake of the tracker, it will be assumed the money received over a year – a projected $2.04 billion – would be distributed evenly.
The tracker presumes that Medicaid expansion would begin in Mississippi on July 1 – the first day of a new fiscal year.
It’s also helpful to explain how the University Research Center derived the projection the state would receive $2.04 billion the first year in federal funds for expanding Medicaid.
The bulk of the federal funds would come from taking the projected number of enrollees – nearly 250,000 — and multiplying that number by the estimated $6,139 expenditure per enrollee. The federal government pays 90% of that cost.
Included in that is money the state would receive by moving certain groups of people currently enrolled in Medicaid where the federal government pays 77.3% of the costs to the new expansion population where the federal government pays 90% of the costs.
In addition, the state would receive funds from the federal government paying a tax to the state – a 3% insurance tax on each new expansion enrollee.
And during the first two years of expansion, the state would receive an estimated $335.4 million in new funds the first year of expansion and an estimated $345.5 million in new funds the second year. The funds would be provided to the state as an incentive to expand Medicaid as 40 other states have done.
The amount of the incentive funds to expand Medicaid is derived by adding 5% to the federal match the state receives from the federal government for the traditional Medicaid program. The federal match Mississippi receives for the traditional Medicaid program is 77.3%. In other words, for every dollar spent on Medicaid, the federal government pays 77.3 cents. Mississippi receives the highest federal match for the traditional Medicaid program of any state in the nation because of multiple reasons, such as the state’s high poverty rate. If Mississippi expanded Medicaid, the federal match non-expansion enrollees would go to 82.3% for two years, resulting in $680 million to the state over two years.
After two years, the 5% increase in the federal match for the traditional Medicaid program would go away. With the removal of the 5% enhanced match, the University Research Center projects the total federal expenditure on Medicaid expansion would drop to $1.78 billion in year three.
At that point, if Medicaid is not expanded, Mississippi Today will have to recalculate its tracker.
This article first appeared on Mississippi Today and is republished here under a Creative Commons license.![]()
Did you miss our previous article…
https://www.biloxinewsevents.com/?p=373719
Mississippi Today
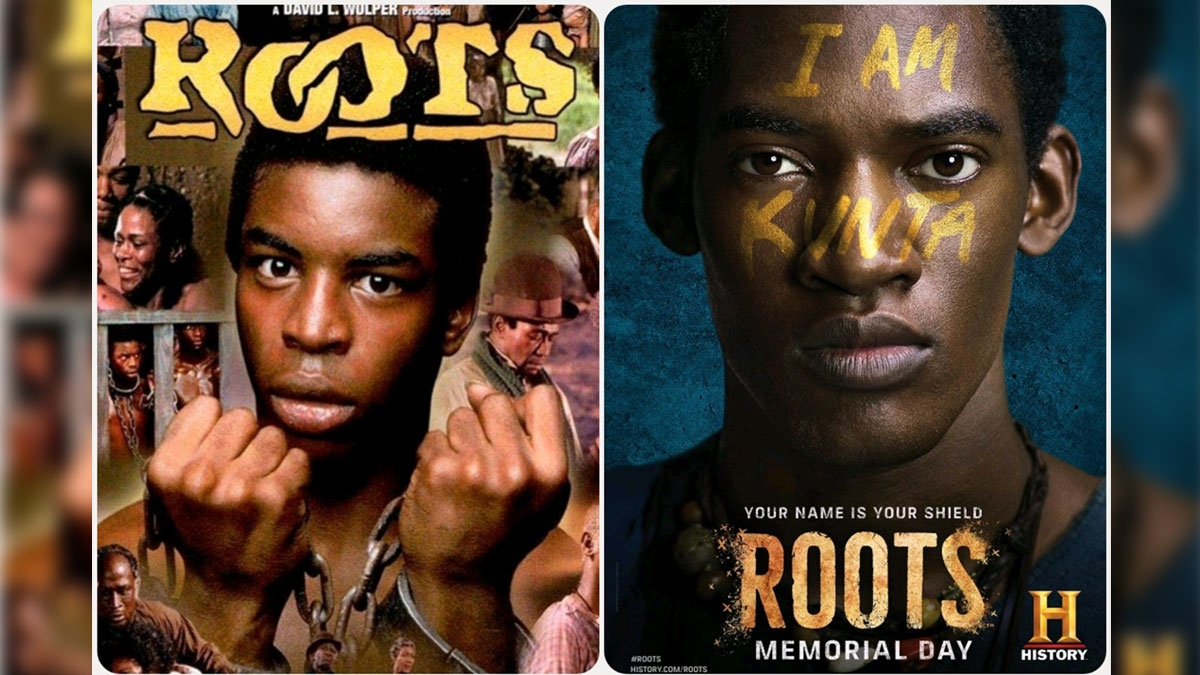
On this day in 1977, Alex Haley awarded Pulitzer for ‘Roots’
April 19, 1977

Alex Haley was awarded a special Pulitzer Prize for “Roots,” which was also adapted for television.
Network executives worried that the depiction of the brutality of the slave experience might scare away viewers. Instead, 130 million Americans watched the epic miniseries, which meant that 85% of U.S. households watched the program.
The miniseries received 36 Emmy nominations and won nine. In 2016, the History Channel, Lifetime and A&E remade the miniseries, which won critical acclaim and received eight Emmy nominations.
This article first appeared on Mississippi Today and is republished here under a Creative Commons Attribution-NoDerivatives 4.0 International License.![]()
Mississippi Today
Speaker White wants Christmas tree projects bill included in special legislative session

House Speaker Jason White sent a terse letter to Lt. Gov. Delbert Hosemann on Thursday, saying House leaders are frustrated with Senate leaders refusing to discuss a “Christmas tree” bill spending millions on special projects across the state.
The letter signals the two Republican leaders remain far apart on setting an overall $7 billion state budget. Bickering between the GOP leaders led to a stalemate and lawmakers ending their regular 2025 session without setting a budget. Gov. Tate Reeves plans to call them back into special session before the new budget year starts July 1 to avoid a shutdown, but wants them to have a budget mostly worked out before he does so.
White’s letter to Hosemann, which contains words in all capital letters that are underlined and italicized, said that the House wants to spend cash reserves on projects for state agencies, local communities, universities, colleges, and the Mississippi Department of Transportation.
“We believe the Senate position to NOT fund any local infrastructure projects is unreasonable,” White wrote.
The speaker in his letter noted that he and Hosemann had a meeting with the governor on Tuesday. Reeves, according to the letter, advised the two legislative leaders that if they couldn’t reach an agreement on how to disburse the surplus money, referred to as capital expense money, they should not spend any of it on infrastructure.
A spokesperson for Hosemann said the lieutenant governor has not yet reviewed the letter, and he was out of the office on Thursday working with a state agency.
“He is attending Good Friday services today, and will address any correspondence after the celebration of Easter,” the spokesperson said.
Hosemann has recently said the Legislature should set an austere budget in light of federal spending cuts coming from the Trump administration, and because state lawmakers this year passed a measure to eliminate the state income tax, the source of nearly a third of the state’s operating revenue.
Lawmakers spend capital expense money for multiple purposes, but the bulk of it — typically $200 million to $400 million a year — goes toward local projects, known as the Christmas Tree bill. Lawmakers jockey for a share of the spending for their home districts, in a process that has been called a political spoils system — areas with the most powerful lawmakers often get the largest share, not areas with the most needs. Legislative leaders often use the projects bill as either a carrot or stick to garner votes from rank and file legislators on other issues.
A Mississippi Today investigation last year revealed House Ways and Means Chairman Trey Lamar, a Republican from Sentobia, has steered tens of millions of dollars in Christmas tree spending to his district, including money to rebuild a road that runs by his north Mississippi home, renovate a nearby private country club golf course and to rebuild a tiny cul-de-sac that runs by a home he has in Jackson.
There is little oversight on how these funds are spent, and there is no requirement that lawmakers disburse the money in an equal manner or based on communities’ needs.
In the past, lawmakers borrowed money for Christmas tree bills. But state coffers have been full in recent years largely from federal pandemic aid spending, so the state has been spending its excess cash. White in his letter said the state has “ample funds” for a special projects bill.
“We, in the House, would like to sit down and have an agreement with our Senate counterparts on state agency Capital Expenditure spending AND local projects spending,” White wrote. “It is extremely important to our agencies and local governments. The ball is in your court, and the House awaits your response.”
This article first appeared on Mississippi Today and is republished here under a Creative Commons Attribution-NoDerivatives 4.0 International License.
Mississippi Today
Advocate: Election is the chance for Jackson to finally launch in the spirit of Blue Origin

Editor’s note: This essay is part of Mississippi Today Ideas, a platform for thoughtful Mississippians to share fact-based ideas about our state’s past, present and future. You can read more about the section here.
As the world recently watched the successful return of Blue Origin’s historic all-women crew from space, Jackson stands grounded. The city is still grappling with problems that no rocket can solve.
But the spirit of that mission — unity, courage and collective effort — can be applied right here in our capital city. Instead of launching away, it is time to launch together toward a more just, functioning and thriving Jackson.
The upcoming mayoral runoff election on April 22 provides such an opportunity, not just for a new administration, but for a new mindset. This isn’t about endorsements. It’s about engagement.
It’s a moment for the people of Jackson and Hinds County to take a long, honest look at ourselves and ask if we have shown up for our city and worked with elected officials, instead of remaining at odds with them.
It is time to vote again — this time with deeper understanding and shared responsibility. Jackson is in crisis — and crisis won’t wait.
According to the U.S. Census projections, Jackson is the fastest-shrinking city in the United States, losing nearly 4,000 residents in a single year. That kind of loss isn’t just about numbers. It’s about hope, resources, and people’s decision to give up rather than dig in.
Add to that the long-standing issues: a crippled water system, public safety concerns, economic decline and a sense of division that often pits neighbor against neighbor, party against party and race against race.
Mayor Chokwe Antar Lumumba has led through these storms, facing criticism for his handling of the water crisis, staffing issues and infrastructure delays. But did officials from the city, the county and the state truly collaborate with him or did they stand at a distance, waiting to assign blame?
On the flip side, his runoff opponent, state Sen. John Horhn, who has served for more than three decades, is now seeking to lead the very city he has represented from the Capitol. Voters should examine his legislative record and ask whether he used his influence to help stabilize the administration or only to position himself for this moment.
Blaming politicians is easy. Building cities is hard. And yet that is exactly what’s needed. Jackson’s future will not be secured by a mayor alone. It will take so many of Jackson’s residents — voters, business owners, faith leaders, students, retirees, parents and young people — to move this city forward. That’s the liftoff we need.
It is time to imagine Jackson as a capital city where clean, safe drinking water flows to every home — not just after lawsuits or emergencies, but through proactive maintenance and funding from city, state and federal partnerships. The involvement of the U.S. Environmental Protection Agency in the effort to improve the water system gives the city leverage.
Public safety must be a guarantee and includes prevention, not just response, with funding for community-based violence interruption programs, trauma services, youth job programs and reentry support. Other cities have done this and it’s working.
Education and workforce development are real priorities, preparing young people not just for diplomas but for meaningful careers. That means investing in public schools and in partnerships with HBCUs, trade programs and businesses rooted right here.
Additionally, city services — from trash collection to pothole repair — must be reliable, transparent and equitable, regardless of zip code or income. Seamless governance is possible when everyone is at the table.
Yes, democracy works because people show up. Not just to vote once, but to attend city council meetings, serve on boards, hold leaders accountable and help shape decisions about where resources go.
This election isn’t just about who gets the title of mayor. It’s about whether Jackson gets another chance at becoming the capital city Mississippi deserves — a place that leads by example and doesn’t lag behind.
The successful Blue Origin mission didn’t happen by chance. It took coordinated effort, diverse expertise and belief in what was possible. The same is true for this city.
We are not launching into space. But we can launch a new era marked by cooperation over conflict, and by sustained civic action over short-term outrage.
On April 22, go vote. Vote not just for a person, but for a path forward because Jackson deserves liftoff. It starts with us.
Pauline Rogers is a longtime advocate for criminal justice reform and the founder of the RECH Foundation, an organization dedicated to supporting formerly incarcerated individuals as they reintegrate into society. She is a Transformative Justice Fellow through The OpEd Project Public Voices Fellowship.
This article first appeared on Mississippi Today and is republished here under a Creative Commons Attribution-NoDerivatives 4.0 International License.![]()
-

 Mississippi Today6 days ago
Mississippi Today6 days agoLawmakers used to fail passing a budget over policy disagreement. This year, they failed over childish bickering.
-

 Mississippi Today6 days ago
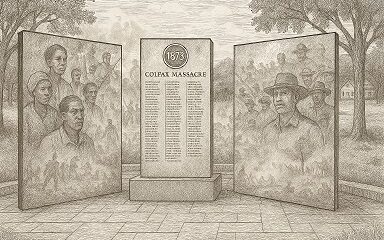
Mississippi Today6 days agoOn this day in 1873, La. courthouse scene of racial carnage
-

 Local News6 days ago
Local News6 days agoSouthern Miss Professor Inducted into U.S. Hydrographer Hall of Fame
-

 News from the South - Alabama News Feed5 days ago
News from the South - Alabama News Feed5 days agoFoley man wins Race to the Finish as Kyle Larson gets first win of 2025 Xfinity Series at Bristol
-

 News from the South - Alabama News Feed5 days ago
News from the South - Alabama News Feed5 days agoFederal appeals court upholds ruling against Alabama panhandling laws
-

 News from the South - Florida News Feed7 days ago
News from the South - Florida News Feed7 days agoSevere weather has come and gone for Central Florida, but the rain went with it
-

 News from the South - Alabama News Feed7 days ago
News from the South - Alabama News Feed7 days agoBellingrath Gardens previews its first Chinese Lantern Festival
-

 News from the South - Texas News Feed6 days ago
News from the South - Texas News Feed6 days ago1 dead after 7 people shot during large gathering at Crosby gas station, HCSO says