Mississippi Today
Nearly 1 in 4 adults dumped from Medicaid are now uninsured, survey finds
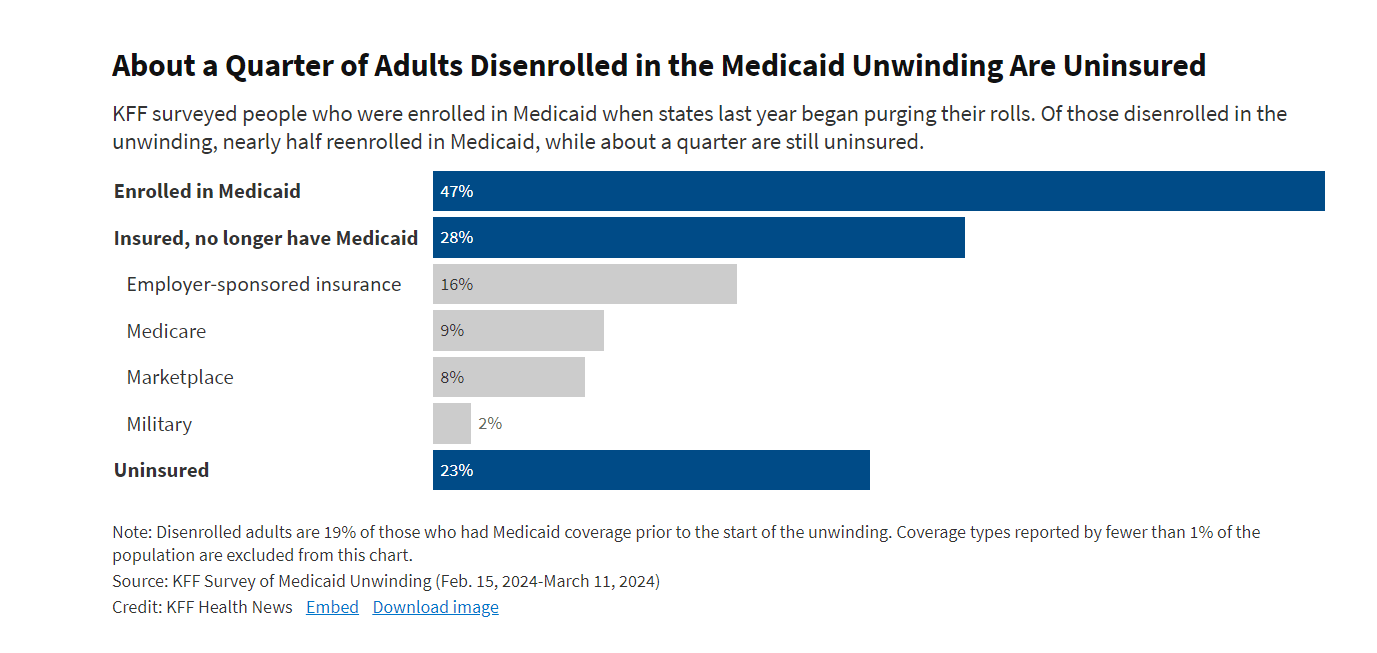
Nearly a quarter of adults disenrolled from Medicaid in the past year say they are now uninsured, according to a survey released Friday that details how tens of millions of Americans struggled to retain coverage in the government insurance program for low-income people after pandemic-era protections began expiring last spring.
The first national survey of adults whose Medicaid eligibility was reviewed during the unwinding found nearly half of people who lost their government coverage signed back up weeks or months later — suggesting they should never have been dropped in the first place.
While 23% reported being uninsured, an additional 28% found other coverage — through an employer, Medicare, the Affordable Care Act’s insurance marketplace, or health care for members of the military, the survey by KFF found.
“Twenty-three percent is a striking number especially when you think about the number of people who lost Medicaid coverage,” said Chima Ndumele, an associate professor of health policy at the Yale University School of Public Health.
Going without insurance even for a short period of time can lead people to delay seeking care and leave them at financial risk when they do.
Seven in 10 adults who were disenrolled during the unwinding process say they became uninsured at least temporarily when they lost their Medicaid coverage.
Adrienne Hamar, 49, of Plymouth Meeting, Pennsylvania, said she struggled to enroll in an Affordable Care Act marketplace plan this winter after the state informed her that she and her two children no longer qualified for Medicaid. They had been enrolled since 2020. She said phone lines were busy at the state’s marketplace and she couldn’t complete the process online.

Hamar, who works as a home health aide, and her children were uninsured in March. But since April 1, they’ve been enrolled in a marketplace plan that, with the help of government subsidies, costs $50 a month for the family.
“I was very relieved,” she said. Unsure of their insurance status, Hamar said, her 23-year-old daughter delayed getting a dental checkup.
Hamar’s struggles were common, the survey found.
Of adults enrolled in Medicaid before the unwinding, about 35% who tried to renew their coverage described the process as difficult, and about 48% said it was at least somewhat stressful.
About 56% of those disenrolled say they skipped or delayed care or prescriptions while attempting to renew their Medicaid coverage.
“People’s current insurance status is likely to be very much in flux, and we would expect at least some of the people who say they are currently uninsured to reenroll in Medicaid — many say they are still trying — or enroll in other coverage within a short period of time,” said Jennifer Tolbert, a co-author of the KFF report and the director of KFF’s State Health Reform and Data Program.
The survey didn’t include children, and the KFF researchers said their findings therefore couldn’t be extrapolated to determine how the Medicaid unwinding has affected the overall U.S. uninsured rate, which hit a record low of 7.7% in early 2023. Nearly half of enrollees in Medicaid and the related Children’s Health Insurance Program are children.
The unwinding, in which states are reassessing eligibility for Medicaid among millions of Americans who enrolled before or during the pandemic and dropping those who no longer qualify or did not complete the renewal process, won’t be completed until later this year. Enrollment in Medicaid and CHIP grew to a record of nearly 94.5 million in April of last year, three years after the federal government prohibited states from cutting people from their rolls during the covid-19 public health emergency.
Nationally, states have disenrolled about 20 million people from Medicaid in the past year, most of them for procedural reasons such as failure to submit required paperwork. That number is expected to grow, as states have a few more months to redetermine enrollees’ eligibility.
Among adults who had Medicaid prior to the start of the unwinding, 83% retained their coverage or reenrolled, while 8% found other insurance and 8% were uninsured. The share left uninsured was larger in states that have not expanded Medicaid under the ACA (17%) than in states that have (6%). Forty states have expanded Medicaid to cover everyone with an income under 138% of the federal poverty rate, or $31,200 for a family of four this year.
The KFF survey found that nearly 1 in 3 disenrolled adults discovered only when they sought health care — such as going to a doctor or a pharmacy — that they had been dropped from Medicaid.

Indira Navas of Miami found out that her 6-year-old son, Andres, had been disenrolled from Florida’s Medicaid program when she took him to a doctor appointment in March. She had scheduled Andres’ appointment months in advance and is frustrated that he remains uninsured and his therapy for anxiety and hyperactivity has been disrupted.
Navas said the state could not explain why her 12-year-old daughter, Camila, remained covered by Medicaid even though the children live in the same household with their parents.
“It doesn’t make sense that they would cover one of my children and not the other,” she said.
Kate McEvoy, executive director of the National Association of Medicaid Directors, said the sheer volume of millions of people being redetermined for eligibility has overwhelmed some state call centers trying to support enrollees.
She said states have tried many ways to communicate with enrollees, including through public outreach campaigns, text, email, and apps. “Until the moment your coverage is at stake, it’s hard to penetrate people’s busy lives,” she said.
The KFF survey, of 1,227 adults who had Medicaid coverage in early 2023 prior to the start of the unwinding on April 1, 2023, was conducted between Feb. 15, 2024, and March 11, 2024. The margin of sampling error was plus or minus 4 percentage points.
KFF Health News correspondent Daniel Chang contributed to this article.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
This article first appeared on Mississippi Today and is republished here under a Creative Commons license.![]()
Did you miss our previous article…
https://www.biloxinewsevents.com/?p=348953
Mississippi Today
Early voting proposal killed on last day of Mississippi legislative session
Mississippi will remain one of only three states without no-excuse early voting or no-excuse absentee voting.
Senate leaders, on the last day of their regular 2025 session, decided not to send a bill to Gov. Tate Reeves that would have expanded pre-Election Day voting options. The governor has been vocally opposed to early voting in Mississippi, and would likely have vetoed the measure.
The House and Senate this week overwhelmingly voted for legislation that established a watered-down version of early voting. The proposal would have required voters to go to a circuit clerk’s office and verify their identity with a photo ID.
The proposal also listed broad excuses that would have allowed many voters an opportunity to cast early ballots.
The measure passed the House unanimously and the Senate approved it 42-7. However, Sen. Jeff Tate, a Republican from Meridian who strongly opposes early voting, held the bill on a procedural motion.
Senate Elections Chairman Jeremy England chose not to dispose of Tate’s motion on Thursday morning, the last day the Senate was in session. This killed the bill and prevented it from going to the governor.
England, a Republican from Vancleave, told reporters he decided to kill the legislation because he believed some of its language needed tweaking.
The other reality is that Republican Gov. Tate Reeves strongly opposes early voting proposals and even attacked England on social media for advancing the proposal out of the Senate chamber.
England said he received word “through some sources” that Reeves would veto the measure.
“I’m not done working on it, though,” England said.
Although Mississippi does not have no-excuse early voting or no-excuse absentee voting, it does have absentee voting.
To vote by absentee, a voter must meet one of around a dozen legal excuses, such as temporarily living outside of their county or being over 65. Mississippi law doesn’t allow people to vote by absentee purely out of convenience or choice.
Several conservative states, such as Texas, Louisiana, Arkansas and Florida, have an in-person early voting system. The Republican National Committee in 2023 urged Republican voters to cast an early ballot in states that have early voting procedures.
Yet some Republican leaders in Mississippi have ardently opposed early voting legislation over concerns that it undermines election security.
This article first appeared on Mississippi Today and is republished here under a Creative Commons license.
.
Mississippi Today
Mississippi Legislature approves DEI ban after heated debate
Mississippi lawmakers have reached an agreement to ban diversity, equity and inclusion programs and a list of “divisive concepts” from public schools across the state education system, following the lead of numerous other Republican-controlled states and President Donald Trump’s administration.
House and Senate lawmakers approved a compromise bill in votes on Tuesday and Wednesday. It will likely head to Republican Gov. Tate Reeves for his signature after it clears a procedural motion.
The agreement between the Republican-dominated chambers followed hours of heated debate in which Democrats, almost all of whom are Black, excoriated the legislation as a setback in the long struggle to make Mississippi a fairer place for minorities. They also said the bill could bog universities down with costly legal fights and erode academic freedom.
Democratic Rep. Bryant Clark, who seldom addresses the entire House chamber from the podium during debates, rose to speak out against the bill on Tuesday. He is the son of the late Robert Clark, the first Black Mississippian elected to the state Legislature since the 1800s and the first Black Mississippian to serve as speaker pro tempore and preside over the House chamber since Reconstruction.
“We are better than this, and all of you know that we don’t need this with Mississippi history,” Clark said. “We should be the ones that say, ‘listen, we may be from Mississippi, we may have a dark past, but you know what, we’re going to be the first to stand up this time and say there is nothing wrong with DEI.'”
Legislative Republicans argued that the measure — which will apply to all public schools from the K-12 level through universities — will elevate merit in education and remove a list of so-called “divisive concepts” from academic settings. More broadly, conservative critics of DEI say the programs divide people into categories of victims and oppressors and infuse left-wing ideology into campus life.
“We are a diverse state. Nowhere in here are we trying to wipe that out,” said Republican Sen. Tyler McCaughn, one of the bill’s authors. “We’re just trying to change the focus back to that of excellence.”
The House and Senate initially passed proposals that differed in who they would impact, what activities they would regulate and how they aim to reshape the inner workings of the state’s education system. Some House leaders wanted the bill to be “semi-vague” in its language and wanted to create a process for withholding state funds based on complaints that almost anyone could lodge. The Senate wanted to pair a DEI ban with a task force to study inefficiencies in the higher education system, a provision the upper chamber later agreed to scrap.
The concepts that will be rooted out from curricula include the idea that gender identity can be a “subjective sense of self, disconnected from biological reality.” The move reflects another effort to align with the Trump administration, which has declared via executive order that there are only two sexes.
The House and Senate disagreed on how to enforce the measure but ultimately settled on an agreement that would empower students, parents of minor students, faculty members and contractors to sue schools for violating the law.
People could only sue after they go through an internal campus review process and a 25-day period when schools could fix the alleged violation. Republican Rep. Joey Hood, one of the House negotiators, said that was a compromise between the chambers. The House wanted to make it possible for almost anyone to file lawsuits over the DEI ban, while Senate negotiators initially bristled at the idea of fast-tracking internal campus disputes to the legal system.
The House ultimately held firm in its position to create a private cause of action, or the right to sue, but it agreed to give schools the ability to conduct an investigative process and potentially resolve the alleged violation before letting people sue in chancery courts.
“You have to go through the administrative process,” said Republican Sen. Nicole Boyd, one of the bill’s lead authors. “Because the whole idea is that, if there is a violation, the school needs to cure the violation. That’s what the purpose is. It’s not to create litigation, it’s to cure violations.”
If people disagree with the findings from that process, they could also ask the attorney general’s office to sue on their behalf.
Under the new law, Mississippi could withhold state funds from schools that don’t comply. Schools would be required to compile reports on all complaints filed in response to the new law.
Trump promised in his 2024 campaign to eliminate DEI in the federal government. One of the first executive orders he signed did that. Some Mississippi lawmakers introduced bills in the 2024 session to restrict DEI, but the proposals never made it out of committee. With the national headwinds at their backs and several other laws in Republican-led states to use as models, Mississippi lawmakers made plans to introduce anti-DEI legislation.
The policy debate also unfolded amid the early stages of a potential Republican primary matchup in the 2027 governor’s race between State Auditor Shad White and Lt. Gov. Delbert Hosemann. White, who has been one of the state’s loudest advocates for banning DEI, had branded Hosemann in the months before the 2025 session “DEI Delbert,” claiming the Senate leader has stood in the way of DEI restrictions passing the Legislature.
During the first Senate floor debate over the chamber’s DEI legislation during this year’s legislative session, Hosemann seemed to be conscious of these political attacks. He walked over to staff members and asked how many people were watching the debate live on YouTube.
As the DEI debate cleared one of its final hurdles Wednesday afternoon, the House and Senate remained at loggerheads over the state budget amid Republican infighting. It appeared likely the Legislature would end its session Wednesday or Thursday without passing a $7 billion budget to fund state agencies, potentially threatening a government shutdown.
“It is my understanding that we don’t have a budget and will likely leave here without a budget. But this piece of legislation …which I don’t think remedies any of Mississippi’s issues, this has become one of the top priorities that we had to get done,” said Democratic Sen. Rod Hickman. “I just want to say, if we put that much work into everything else we did, Mississippi might be a much better place.”
This article first appeared on Mississippi Today and is republished here under a Creative Commons license.
Mississippi Today
House gives Senate 5 p.m. deadline to come to table, or legislative session ends with no state budget
The House on Wednesday attempted one final time to revive negotiations between it and the Senate over passing a state budget.
Otherwise, the two Republican-led chambers will likely end their session without funding government services for the next fiscal year and potentially jeopardize state agencies.
The House on Wednesday unanimously passed a measure to extend the legislative session and revive budget bills that had died on legislative deadlines last weekend.
House Speaker Jason White said he did not have any prior commitment that the Senate would agree to the proposal, but he wanted to extend one last offer to pass the budget. White, a Republican from West, said if he did not hear from the Senate by 5 p.m. on Wednesday, his chamber would end its regular session.
“The ball is in their court,” White said of the Senate. “Every indication has been that they would not agree to extend the deadlines for purposes of doing the budget. I don’t know why that is. We did it last year, and we’ve done it most years.”
But it did not appear likely Wednesday afternoon that the Senate would comply.
The Mississippi Legislature has not left Jackson without setting at least most of the state budget since 2009, when then Gov. Haley Barbour had to force them back to set one to avoid a government shutdown.
The House measure to extend the session is now before the Senate for consideration. To pass, it would require a two-thirds majority vote of senators. But that might prove impossible. Numerous senators on both sides of the aisle vowed to vote against extending the current session, and Lt. Gov. Delbert Hosemann who oversees the chamber said such an extension likely couldn’t pass.
Senate leadership seemed surprised at the news that the House passed the resolution to negotiate a budget, and several senators earlier on Wednesday made passing references to ending the session without passing a budget.
“We’ll look at it after it passes the full House,” Senate President Pro Tempore Dean Kirby said.
The House and Senate, each having a Republican supermajority, have fought over many issues since the legislative session began early January.
But the battle over a tax overhaul plan, including elimination of the state individual income tax, appeared to cause a major rift. Lawmakers did pass a tax overhaul, which the governor has signed into law, but Senate leaders cried foul over how it passed, with the House seizing on typos in the Senate’s proposal that accidentally resembled the House’s more aggressive elimination plan.
The Senate had urged caution in eliminating the income tax, and had economic growth triggers that would have likely phased in the elimination over many years. But the typos essentially negated the triggers, and the House and governor ran with it.
The two chambers have also recently fought over the budget. White said he communicated directly with Senate leaders that the House would stand firm on not passing a budget late in the session.
But Senate leaders said they had trouble getting the House to meet with them to haggle out the final budget.
On the normally scheduled “conference weekend” with a deadline to agree to a budget last Saturday, the House did not show, taking the weekend off. This angered Hosemann and the Senate. All the budget bills died, requiring a vote to extend the session, or the governor forcing them into a special session.
If the Legislature ends its regular session without adopting a budget, the only option to fund state agencies before their budgets expire on June 30 is for Gov. Tate Reeves to call lawmakers back into a special session later.
“There really isn’t any other option (than the governor calling a special session),” Lt. Gov. Delbert Hosemann previously said.
If Reeves calls a special session, he gets to set the Legislature’s agenda. A special session call gives an otherwise constitutionally weak Mississippi governor more power over the Legislature.
This article first appeared on Mississippi Today and is republished here under a Creative Commons license.
-

 Mississippi Today2 days ago
Mississippi Today2 days agoPharmacy benefit manager reform likely dead
-

 News from the South - Virginia News Feed7 days ago
News from the South - Virginia News Feed7 days agoYoungkin removes Ellis, appoints Cuccinelli to UVa board | Virginia
-

 News from the South - Alabama News Feed7 days ago
News from the South - Alabama News Feed7 days agoUniversity of Alabama student detained by ICE moved to Louisiana
-

 News from the South - Oklahoma News Feed5 days ago
News from the South - Oklahoma News Feed5 days agoTornado watch, severe thunderstorm warnings issued for Oklahoma
-

 News from the South - Georgia News Feed5 days ago
News from the South - Georgia News Feed5 days agoGeorgia road project forcing homeowners out | FOX 5 News
-

 News from the South - West Virginia News Feed6 days ago
News from the South - West Virginia News Feed6 days agoHometown Hero | Restaurant owner serves up hope
-

 News from the South - Georgia News Feed6 days ago
News from the South - Georgia News Feed6 days agoBudget cuts: Senior Citizens Inc. and other non-profits worry for the future
-

 News from the South - Kentucky News Feed3 days ago
News from the South - Kentucky News Feed3 days agoTornado practically rips Bullitt County barn in half with man, several animals inside