Mississippi Today
Mississippi remains an outlier in jailing people with serious mental illness without charges
This article contains descriptions of threats of violence and mental illness. If you or someone you know needs help:
- Call the National Suicide Prevention Lifeline: 988
- Text the Crisis Text Line from anywhere in the U.S. to reach a crisis counselor: 741741
This article was produced for ProPublica’s Local Reporting Network in partnership with Mississippi Today. Sign up for Dispatches to get stories like this one as soon as they are published.
Nearly 40 years ago, a federal appeals court ruled that Alabama officials could not jail people in mental health crisis who were sent to the state for help. Jailing people going through the state’s civil commitment process, the court decided, amounted to punishment. And about 30 years ago, after Kentucky was labeled the worst state in the nation for jailing mentally ill people without charges, legislators there banned it.
But a new survey of counties and an analysis of jail dockets in Mississippi, which has no such law, has found that people going through the civil commitment process for mental illness are regularly jailed as they await evaluation and treatment, even when they haven’t been charged with a crime. Some counties routinely hold such people in jail — people awaiting treatment for mental illness or substance abuse were held in jail without charges at least 2,000 times from 2019 to 2022 in 19 counties alone, sometimes for days or weeks.
Nationally, Mississippi is a stark outlier. Mississippi Today and ProPublica conducted a nationwide survey of disability advocacy organizations and state agencies that oversee behavioral health. None described anything close to the scale of what’s happening in Mississippi.
Civil commitment laws are meant to ensure people get treatment even when they don’t recognize that they need it, said James Tucker, an attorney and the director of the Alabama Disabilities Advocacy Program. Locking them up as they wait for a treatment bed doesn’t fulfill that goal.
“The bargain for your lack of freedom is that the state has decided you need treatment,” he said. “The minute that order is entered, the state has a constitutional duty to deliver treatment.”
At least 12 states plus the District of Columbia prohibit jailing people undergoing commitment proceedings for mental illness unless they have been charged with a crime.
Mississippi law, however, allows people going through the civil commitment process to be sent to jail if there is “no reasonable alternative.” If there are no publicly funded beds in appropriate facilities, local officials sometimes decide they have no other option.
“We Forbid the Use of Jails”
In the 1970s, a federal class-action lawsuit against Alabama officials alleged that it was unconstitutional to jail people going through the commitment process for mental illness while they awaited hearings. It was common at the time: Probate judges in three-quarters of the state’s counties had jailed people, according to discovery findings cited in a court ruling.
Lawyers for the plaintiffs — everyone in the state who had been committed or would be in the future — cited previous lawsuits that had uncovered fire hazards, overcrowding and a dearth of mental health and routine medical care in Alabama’s county jails.
The district court ruled against the plaintiffs’ constitutional claims, reasoning that if the local jail was the only option in a county, it was the least restrictive facility that would also protect society.
“The bargain for your lack of freedom is that the state has decided you need treatment. The minute that order is entered, the state has a constitutional duty to deliver treatment.”
James Tucker, director of the Alabama Disabilities Advocacy Program
But in 1984, a panel of judges on the 11th U.S. Circuit Court of Appeals rejected that reasoning. Circuit Judge Thomas Alonzo Clark wrote in his opinion that nothing prevented counties from placing people in a public facility in another county or in a local private facility that was equipped to handle mentally ill patients.
Clark cited a doctor’s testimony that jail often worsened psychosis, made it harder to treat people and increased suicidal tendencies.
“We forbid the use of jails for the purpose of detaining persons awaiting involuntary civil commitment proceedings, finding that to do so violates those persons’ substantive and procedural due process rights,” the judge wrote.
The reasons that Alabama officials provided for placing people in jail were similar to Mississippi officials’ arguments today. But Mississippi is in a different federal circuit, and the practice there has not been tested with a class-action lawsuit.
A sister of one woman who had died in a Mississippi jail in 1987 tried and failed to convince a federal judge that the woman’s rights had been violated when she was incarcerated without treatment.
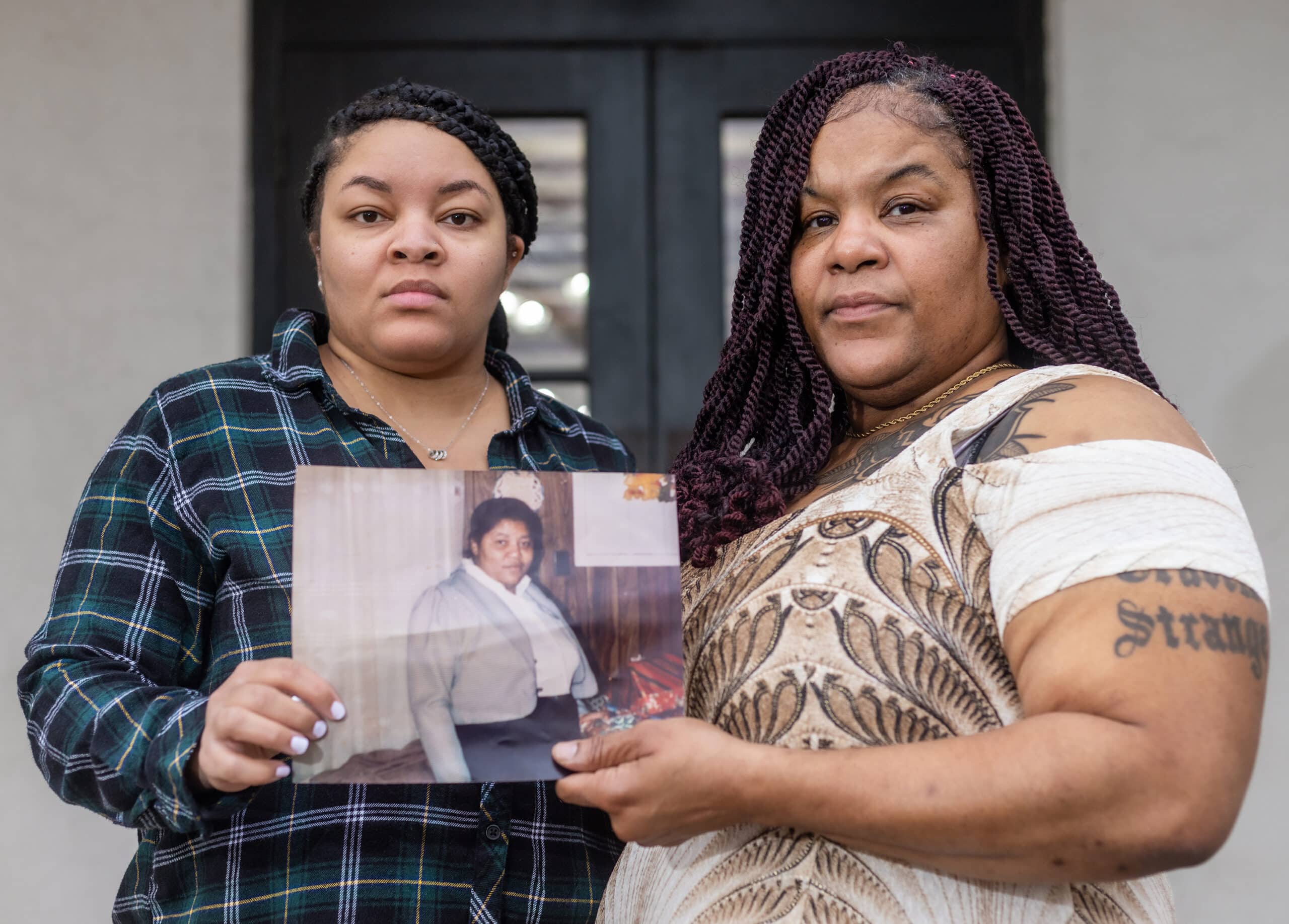
Mae Evelyn Boston, an Oxford woman who had dealt with paranoid schizophrenia for most of her adult life, had a psychotic episode shortly after giving birth. Her older daughter, Everlean, was 12 years old; she remembers her mother saying she was going to kill the baby because the girl “had a demon in her.”
One of Boston’s sisters initiated commitment proceedings — making Boston one of more than 100 people jailed for that reason from 1984 to 1988 in Lafayette County, according to a deposition cited in a 1990 ruling by U.S. District Judge Neal Biggers. When deputies arrived to take her mother into custody for evaluation, Everlean recalled, it took six of them to get her onto the ground before handcuffing her and placing her in the back of a cop car.
Once Boston was in jail, guards did not complete a medical screening required by department policy and didn’t know Boston had given birth via cesarean section 12 days before, Biggers wrote. She died two days later from heart failure caused by blood clots.
Everlean Boston remembers her mother smoking cigarettes and listening to the blues on quiet Sundays at home. The day deputies took her mother away was the last time she saw her. “I never got to say goodbye,” she recalled. “I never got to say I loved her. It hurts.”
“I never got to say goodbye. I never got to say I loved her. It hurts.”
Everlean Boston, whose mother, Mae Evelyn Boston, died in jail as she went through the civil commitment process
Biggers concluded that the “medical care customarily provided by the county for mentally ill detainees does not fall below constitutional standards” and that what happened with Boston represented a “scheduling error” and an “isolated instance.” The county, which argued it had provided adequate care for Boston, had the right to detain people like her “in the interest of societal safety,” he found, and those people were not entitled to placement in the “least restrictive alternative” such as a hospital. Biggers considered the Alabama appeals court ruling from a few years earlier, but concluded it didn’t apply because it was based on specific facts about that state’s jails.
“The court declines to hold that use of jails for temporary detention of persons awaiting civil commitment proceedings is unconstitutional per se,” Biggers ruled.
Since then, at least nine lawsuits have been filed over the deaths of Mississippians incarcerated during civil commitment proceedings. None of those lawsuits directly challenged the constitutionality of being jailed during the commitment process. The U.S. Supreme Court has not ruled on the matter, academics and attorneys with expertise in civil commitment said.
In the years after Boston’s death, Mississippi continued to stand out.

In 1992, the National Alliance for the Mentally Ill and Public Citizen’s Health Research Group conducted a national survey about the practice of jailing mentally ill people.
Almost a third of city and county jails in Mississippi responded. About 76% of respondents said they detained people who had not been charged with a crime and were awaiting an evaluation, treatment or hospitalization for mental illness. That was the second-highest percentage of any state in the country and far higher than the national average of 29%.
An unnamed Mississippi jail official said in the organizations’ report that jails were a “dumping ground for what nobody else wants.”
The report gave its “Worst State Award” to Kentucky, where 81% of responding jails reported holding people without criminal charges for mental evaluations.
Two years later, Kentucky’s legislature voted unanimously to ban the practice. The state health agency and its federally designated disability rights organization told Mississippi Today and ProPublica that Kentucky jails today are not used to hold people without charges awaiting mental health evaluations.
Few States Compare to Mississippi
Officials with the Mississippi Department of Mental Health emphasize that they do not support the practice of jailing people during the commitment process. But a spokesperson said they “have heard anecdotally from other states regarding challenges of individuals waiting in jail.”
Nationally, even basic data like the number of people committed each year is elusive. After reviewing some of Mississippi Today and ProPublica’s findings, the Treatment Advocacy Center, a national nonprofit that advocates making it easier for people with mental illness to get treatment, started planning a project to understand how often people are jailed without charges during the commitment process across the U.S.
Mississippi Today and ProPublica contacted agencies overseeing mental health and disability advocacy organizations in every state to find out whether Mississippi is an outlier. It is.
Respondents in 42 states and the District of Columbia said they were not aware of people being regularly held in jail without charges during the psychiatric civil commitment process. In a handful of those states, respondents said they had seen it once or twice over the years.
In two states, people can be sent from state psychiatric hospitals to mental health units inside prisons. In a few others, respondents said they had seen people jailed for noncompliance with court-ordered treatment for mental illness or substance abuse.
Respondents in three other states — Alaska, South Dakota and Wyoming — reported that people sometimes are sent to jail to await psychiatric evaluations, but the information they provided suggested that it happens to fewer people, and for a shorter period, than in Mississippi.
In 2018, staffing shortages at the Alaska Psychiatric Institute caused people to be held at the Anchorage Correctional Complex until they could be evaluated. The next year, an Anchorage judge ordered an end to the practice except in the “rarest circumstances,” finding that it had caused “irreparable harm.”
A subsequent settlement declared that jails shouldn’t be used unless no other option was available and that such detentions should be as short as possible.
But detentions do still occasionally happen in the state when people in rural areas await transportation to an evaluation center, said Mark Regan, legal director at the Disability Law Center of Alaska. According to the Alaska Department of Family and Community Services, people awaiting evaluation were held in jail 555 times from mid-2018 through late February 2023.
Across South Dakota, people without charges sometimes have been held in jail during the commitment process, according to law enforcement agencies and Disability Rights South Dakota, but such holds are limited by law to 24 hours; in Mississippi, the vast majority of cases analyzed were for more than 24 hours. The South Dakota Department of Social Services said it doesn’t track how often it happens and declined to answer questions.
And in Wyoming, a person can be held in jail for up to 72 hours on an emergency basis before a hearing, but they must have a mental examination within 24 hours. Such holds in jail have occurred “in very rare circumstances,” according to the state.
Attempts to constrain the use of jails date back at least to 1950, when the federal government sent governors model legislation that limited the incarceration of people for mental illness to “extreme emergency” situations. The National Institute of Mental Health called incarcerating such people “among the worst of current practices.”
Some states adopted the legislation. Mississippi did not.
This article first appeared on Mississippi Today and is republished here under a Creative Commons license.
Mississippi Today
Mississippi River flooding Vicksburg, expected to crest on Monday
Warren County Emergency Management Director John Elfer said Friday floodwaters from the Mississippi River, which have reached homes in and around Vicksburg, will likely persist until early May. Elfer estimated there areabout 15 to 20 roads underwater in the area.
“We’re about half a foot (on the river gauge) from a major flood,” he said. “But we don’t think it’s going to be like in 2011, so we can kind of manage this.”
The National Weather projects the river to crest at 49.5 feet on Monday, making it the highest peak at the Vicksburg gauge since 2020. Elfer said some residents in north Vicksburg — including at the Ford Subdivision as well as near Chickasaw Road and Hutson Street — are having to take boats to get home, adding that those who live on the unprotected side of the levee are generally prepared for flooding.



“There are a few (inundated homes), but we’ve mitigated a lot of them,” he said. “Some of the structures have been torn down or raised. There are a few people that still live on the wet side of the levee, but they kind of know what to expect. So we’re not too concerned with that.”
The river first reached flood stage in the city — 43 feet — on April 14. State officials closed Highway 465, which connects the Eagle Lake community just north of Vicksburg to Highway 61, last Friday.

Elfer said the areas impacted are mostly residential and he didn’t believe any businesses have been affected, emphasizing that downtown Vicksburg is still safe for visitors. He said Warren County has worked with the U.S. Army Corps of Engineers and the Mississippi Emergency Management Agency to secure pumps and barriers.
“Everybody thus far has been very cooperative,” he said. “We continue to tell people stay out of the flood areas, don’t drive around barricades and don’t drive around road close signs. Not only is it illegal, it’s dangerous.”
NWS projects the river to stay at flood stage in Vicksburg until May 6. The river reached its record crest of 57.1 feet in 2011.




This article first appeared on Mississippi Today and is republished here under a Creative Commons Attribution-NoDerivatives 4.0 International License.![]()
Mississippi Today
With domestic violence law, victims ‘will be a number with a purpose,’ mother says
Joslin Napier. Carlos Collins. Bailey Mae Reed.
They are among Mississippi domestic violence homicide victims whose family members carried their photos as the governor signed a bill that will establish a board to study such deaths and how to prevent them.
Tara Gandy, who lost her daughter Napier in Waynesboro in 2022, said it’s a moment she plans to tell her 5-year-old grandson about when he is old enough. Napier’s presence, in spirit, at the bill signing can be another way for her grandson to feel proud of his mother.
“(The board) will allow for my daughter and those who have already lost their lives to domestic violence … to no longer be just a number,” Gandy said. “They will be a number with a purpose.”
Family members at the April 15 private bill signing included Ashla Hudson, whose son Collins, died last year in Jackson. Grandparents Mary and Charles Reed and brother Colby Kernell attended the event in honor of Bailey Mae Reed, who died in Oxford in 2023.
Joining them were staff and board members from the Mississippi Coalition Against Domestic Violence, the statewide group that supports shelters and advocated for the passage of Senate Bill 2886 to form a Domestic Violence Facility Review Board.
The law will go into effect July 1, and the coalition hopes to partner with elected officials who will make recommendations for members to serve on the board. The coalition wants to see appointees who have frontline experience with domestic violence survivors, said Luis Montgomery, public policy specialist for the coalition.
A spokesperson from Gov. Tate Reeves’ office did not respond to a request for comment Friday.
Establishment of the board would make Mississippi the 45th state to review domestic violence fatalities.
Montgomery has worked on passing a review board bill since December 2023. After an unsuccessful effort in 2024, the coalition worked to build support and educate people about the need for such a board.
In the recent legislative session, there were House and Senate versions of the bill that unanimously passed their respective chambers. Authors of the bills are from both political parties.
The review board is tasked with reviewing a variety of documents to learn about the lead up and circumstances in which people died in domestic violence-related fatalities, near fatalities and suicides – records that can include police records, court documents, medical records and more.
From each review, trends will emerge and that information can be used for the board to make recommendations to lawmakers about how to prevent domestic violence deaths.
“This is coming at a really great time because we can really get proactive,” Montgomery said.
Without a board and data collection, advocates say it is difficult to know how many people have died or been injured in domestic-violence related incidents.
A Mississippi Today analysis found at least 300 people, including victims, abusers and collateral victims, died from domestic violence between 2020 and 2024. That analysis came from reviewing local news stories, the Gun Violence Archive, the National Gun Violence Memorial, law enforcement reports and court documents.
Some recent cases the board could review are the deaths of Collins, Napier and Reed.
In court records, prosecutors wrote that Napier, 24, faced increased violence after ending a relationship with Chance Fabian Jones. She took action, including purchasing a firearm and filing for a protective order against Jones.
Jones’s trial is set for May 12 in Wayne County. His indictment for capital murder came on the first anniversary of her death, according to court records.
Collins, 25, worked as a nurse and was from Yazoo City. His ex-boyfriend Marcus Johnson has been indicted for capital murder and shooting into Collins’ apartment. Family members say Collins had filed several restraining orders against Johnson.
Johnson was denied bond and remains in jail. His trial is scheduled for July 28 in Hinds County.
He was a Jackson police officer for eight months in 2013. Johnson was separated from the department pending disciplinary action leading up to immediate termination, but he resigned before he was fired, Jackson police confirmed to local media.
Reed, 21, was born and raised in Michigan and moved to Water Valley to live with her grandparents and help care for her cousin, according to her obituary.
Kylan Jacques Phillips was charged with first degree murder for beating Reed, according to court records. In February, the court ordered him to undergo a mental evaluation to determine if he is competent to stand trial, according to court documents.
At the bill signing, Gandy said it was bittersweet and an honor to meet the families of other domestic violence homicide victims.
“We were there knowing we are not alone, we can travel this road together and hopefully find ways to prevent and bring more awareness about domestic violence,” she said.
This article first appeared on Mississippi Today and is republished here under a Creative Commons Attribution-NoDerivatives 4.0 International License.
Mississippi Today
Court to rule on DeSoto County Senate districts with special elections looming
A federal three-judge panel will rule in coming days on how political power in northwest Mississippi will be allocated in the state Senate and whether any incumbents in the DeSoto County area might have to campaign against each other in November special elections.
The panel, comprised of all George W. Bush-appointed judges, ordered state officials last week to, again, craft a new Senate map for the area in the suburbs of Memphis. The panel has held that none of the state’s prior maps gave Black voters a realistic chance to elect candidates of their choice.
The latest map proposed by the all-Republican State Board of Election Commissioners tweaked only four Senate districts in northwest Mississippi and does not pit any incumbent senators against each other.
The state’s proposal would keep the Senate districts currently held by Sen. Michael McLendon, a Republican from Hernando and Sen. Kevin Blackwell, a Republican from Southaven, in majority-white districts.
But it makes Sen. David Parker’s district a slightly majority-Black district. Parker, a white Republican from Olive Branch, would run in a district with a 50.1% black voting-age population, according to court documents.
The proposal also maintains the district held by Sen. Reginald Jackson, a Democrat from Marks, as a majority-Black district, although it reduces the Black voting age population from 61% to 53%.
Gov. Tate Reeves, Secretary of State Michael Watson, and Attorney General Lynn Fitch comprise the State Board of Election Commissioners. Reeves and Watson voted to approve the plan. But Watson, according to meeting documents, expressed a wish that the state had more time to consider different proposals.
Fitch did not attend the meeting, but Deputy Attorney General Whitney Lipscomb attended in her place. Lipscomb voted against the map, although it is unclear why. Fitch’s office declined to comment on why she voted against the map because it involves pending litigation.
The reason for redrawing the districts is that the state chapter of the NAACP and Black voters in the state sued Mississippi officials for drawing legislative districts in a way that dilutes Black voting power.
The plaintiffs, represented by the ACLU, are likely to object to the state’s newest proposal, and they have until April 29 to file an objection with the court
The plaintiffs have put forward two alternative proposals for the area in the event the judges rule against the state’s plans.
The first option would place McLendon and Blackwell in the same district, and the other would place McLendon and Jackson in the same district.
It is unclear when the panel of judges will issue a ruling on the state’s plan, but they will not issue a ruling until the plaintiffs file their remaining court documents next week.
While the November election is roughly six months away, changing legislative districts across counties and precincts is technical work, and local election officials need time to prepare for the races.
The judges have not yet ruled on the full elections calendar, but U.S. Fifth Circuit Court of Appeals Judge Leslie Southwick said at a hearing earlier this month that the panel was committed have the elections in November.
This article first appeared on Mississippi Today and is republished here under a Creative Commons Attribution-NoDerivatives 4.0 International License.
-

 News from the South - Florida News Feed6 days ago
News from the South - Florida News Feed6 days agoJim talks with Rep. Robert Andrade about his investigation into the Hope Florida Foundation
-

 News from the South - Arkansas News Feed7 days ago
News from the South - Arkansas News Feed7 days agoValerie Storm Tracker
-

 News from the South - Kentucky News Feed7 days ago
News from the South - Kentucky News Feed7 days agoU.S. Supreme Court pauses deportations under wartime law
-

 News from the South - Alabama News Feed4 days ago
News from the South - Alabama News Feed4 days agoPrayer Vigil Held for Ronald Dumas Jr., Family Continues to Pray for His Return | April 21, 2025 | N
-

 Mississippi Today5 days ago
Mississippi Today5 days ago‘Trainwreck on the horizon’: The costly pains of Mississippi’s small water and sewer systems
-

 News from the South - Texas News Feed5 days ago
News from the South - Texas News Feed5 days agoMeteorologist Chita Craft is tracking a Severe Thunderstorm Warning that's in effect now
-

 News from the South - Florida News Feed4 days ago
News from the South - Florida News Feed4 days agoTrump touts manufacturing while undercutting state efforts to help factories
-

 News from the South - Virginia News Feed5 days ago
News from the South - Virginia News Feed5 days agoTaking video of military bases using drones could be outlawed | Virginia