Space medicine professionals in training consult with each other during a simulation exercise. Katya Arquilla
Arian Anderson, University of Colorado Anschutz Medical Campus
In the coming decade, more people will go to space than ever before as human spaceflight enters a new era. NASA, the European Space Agency and other governmental agencies are partnering to develop crewed missions beyond the Moon. At the same time, these agencies are collaborating with private companies using new technologies to drive down the price of space exploration.
Companies such as SpaceX, Blue Origin and Sierra Space have developed vehicles with reusable boosters, automated flight systems and lightweight materials to support these deep space missions. Some even have ambitions of their own to build private space stations, Moon bases or mining operations in the coming decades.
But as these technologies and partnerships rapidly make spaceflight more accessible, new challenges emerge. For one, maintaining the health and performance of an astronaut crew. My team of researchers and educators at the University of Colorado and others around the world are looking to address this issue.
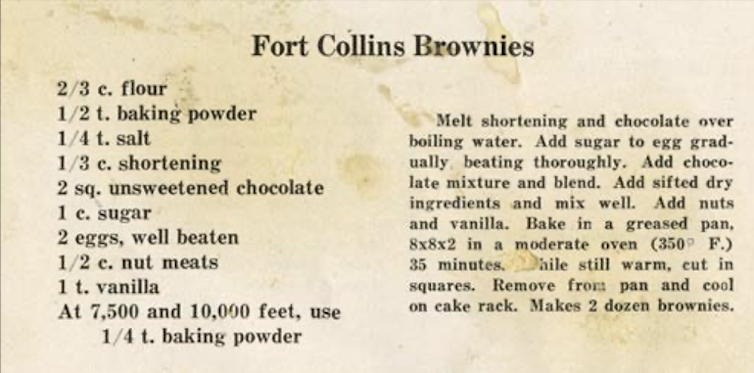
With spaceflight set to expand, astronauts will need access to medical care over longer voyages and on commercial flights. Katya Arquilla
Emerging medical challenges in space
NASA astronauts are some of the most accomplished people on the planet, and they’re some of the healthiest. Astronauts undergo extensive medical and psychological testing that in one study disqualified 26% of final-round applicants. This rigorous screening and testing process effectively limits the chance of a medical event occurring during a mission.
But as spaceflight becomes more accessible, astronaut crews on commercial missions will likely make up the majority of space travelers in the coming years. Private missions will be short and stay in a close orbit around Earth in the near term, but private crews will likely have less training and more chronic medical conditions than the professional astronauts currently living and working in space.
While experiments aboard the International Space Station have extensively studied the normal physiological changes occurring to the human system in weightlessness, there is limited to no data about how common chronic diseases such as diabetes or high blood pressure behave in the space environment.
During Mars missions, astronauts will be away from Earth for long periods of time, with limited access to medical resources.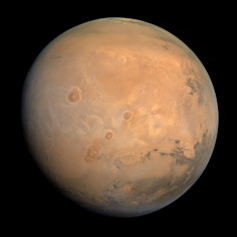
This industry boom is also creating opportunities for long-duration missions to the Moon and Mars. Because of the length of missions and the distance from Earth, professional astronauts on these missions will experience prolonged weightlessness, leading to bone and muscle loss, communication delays of a few seconds up to 40 minutes, and extreme isolation for months to years at a time.
Crews must function autonomously, while being exposed to new hazards such as lunar or Martian dust. Because of the fuel required for these missions, resources will be limited to the lowest mass and volume possible.
As a result, mission planners will need to make difficult decisions to determine what supplies are truly necessary in advance, with limited or unavailable resupply opportunities for food, water and medicine. In space, for example, radiation and humidity inside a spacecraft can cause medications to deteriorate more quickly and become unavailable or even toxic to crew members.
Crews on the space station have access to a flight surgeon at Mission Control to help manage medical care in the same way telehealth is used on Earth. Crews on distant planets, however, will need to perform medical care or procedures autonomously.
In the event of a medical emergency, crews may not be able to evacuate to Earth. Unlike the space station, where medical evacuations to Earth can occur in less than 24 hours, lunar evacuations may take weeks. Evacuations from Mars may not be possible for months or even years.
Put simply, the current approaches to medical care in spaceflight will not meet the needs of future commercial and professional astronauts. Researchers will need to develop new technologies and novel training approaches to prepare future providers to treat medical conditions in space.
The current leaders in space medicine are either experts in aerospace engineering or in medicine, but rarely do experts have formal training or a complete understanding of both fields. And these disciplines often can’t speak each other’s language both literally and figuratively.
Training the next generation
To meet the evolving demands of human spaceflight, educators and universities are looking to develop a way to train specialists who understand both the limitations of the human body and the constraints of engineering design.
Some schools and hospitals, such as the University of Texas Medical Branch, have residency training programs for medical school graduates in aerospace medicine. Others, such as UCLA and Massachusetts General Hospital, have specialty training programs in space medicine, but these currently target fully trained emergency medicine physicians.
My team at the University of Colorado has created a program that integrates human physiology and engineering principles to train medical students to think like engineers.
The University of Colorado brings students to the desert to simulate a lunar base. Students work together to solve simulated medical issues that might occur during a space mission. Katya Arquilla
This program aims to help students understand human health and performance in the spaceflight environment. It approaches these topics from an engineering design and constraints perspective to find solutions to the challenges astronauts will face.
One of our most popular classes is called Mars in Simulated Surface Environments. This class puts students through engineering and medical scenarios in a simulated Mars environment in the Utah desert. Students deal with the challenges of working and providing care while wearing a spacesuit and on a desolate Mars-like landscape.
The stress of the simulations can feel real to the students, and they learn to apply their combined skill sets to care for their fellow crew members.
Educational programs like these and others aim to create cross-trained specialists who understand both patient care and the procedural nature of engineering design and can merge the two, whether for space tourists in orbit or as a pioneer to the surface of another planet.
A new period of spaceflight is here, and these programs are already training experts to make space accessible and safe.![]()
Arian Anderson, Emergency Medicine Physician, University of Colorado Anschutz Medical Campus
This article is republished from The Conversation under a Creative Commons license. Read the original article.