Negotiations to reduce drug prices can sometimes shift costs onto consumers.
C. Michael White, University of Connecticut
When it comes to drug pricing, the Trump and Biden-Harris administrations both have some very modest wins to tout.
As director of the Health Outcomes, Policy, and Evidence Synthesis group at the University of Connecticut School of Pharmacy, I teach and study about the ethics of prescription drug prices and the complexities of drug pricing nationally.
Delving into the presidential candidates’ successes on a number of drug-pricing policies, you’ll see a continuation of progress across the administrations. Neither the Trump administration nor the Biden-Harris administration, however, has done anything to truly lower drug prices for the majority of Americans.
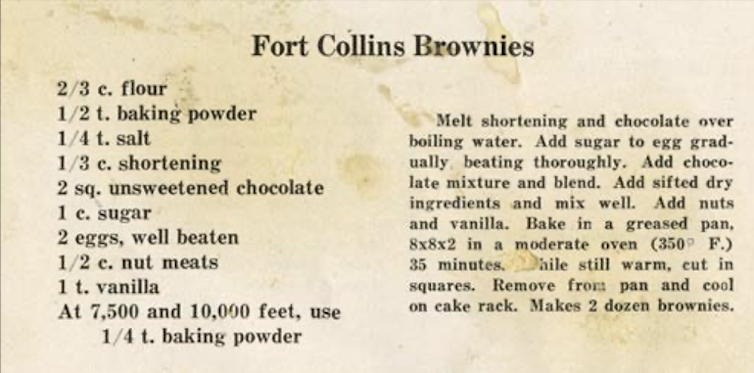
$35 insulin
Insulin is a necessity for patients with diabetes. But from January 2014 to April 2019, the average price per unit went from US$0.22 to $0.34 before dropping back slightly by July 2023 to $0.29 per unit. Since dosing is weight-based, insulin costs for someone weighing 154 pounds would have risen from $231 to $357 a month from 2014 to 2019 and dropped to $305 a month by 2023. Price increases have led some patients to space out their medications by taking less than the dose they need for good blood sugar control. One study estimated that over 25% of patients in an urban diabetes center were underusing their insulin.
In July 2020, the Trump administration enacted a $35 cap on insulin copayments via executive order. In effect, it made participating Medicare Part D programs limit the price of just one of each type of insulin product to $35. For instance, if there were six short-acting insulin products on an insurance plan’s approved drug list, the insurer had to offer one vial form and one pen form at $35.
These price changes did not go into effect during Trump’s presidency. By 2022, only about 800,000 people – or around 11% of the more than 7.4 million people in the U.S. who use insulin to regulate their blood sugar – saw their prices reduced.
Millions of Americans need insulin to manage their diabetes.
In August 2022, the Biden-Harris administration signed the Inflation Reduction Act into law. This maintained the $35 insulin cap with the same stipulations but made the program mandatory for all Medicare Part D and Medicare Part B members. This expanded the number of people who could benefit from cheaper insulin to 3.3 million.
This still doesn’t help a majority of diabetics. If you don’t have Medicare, the $35 reduction does not apply to you. Furthermore, pharmaceutical companies are not responsible for lowering insulin costs under these policies, but health plans are on the hook for lowering copayments. Costs could be passed along to beneficiaries in future Medicare premiums.
Importing Canadian drugs
Americans pay nearly 2.6 times more for prescription drugs than people in other high-income countries. One way regulators have tried to reduce prices is to simply import drugs at the prices pharmaceutical companies charge those countries rather than those charged to U.S. consumers.
In July 2019, the Trump administration proposed importing drugs from Canada as a way to share Canadians’ lower drug costs with American consumers. He signed an executive order allowing the Food and Drug Administration to create the rules under which states could import the drugs. When President Joe Biden came into office, he left the executive order in place and the rulemaking process continued.
Some Americans have traveled across borders for cheaper medications.
No state under the Trump or Biden-Harris administrations has yet been able to successfully import a Canadian drug product. In January 2024, however, the Food and Drug Administration approved Florida’s plan to import Canadian drugs, the first state to receive the green light. Colorado, New Hampshire, New Mexico and Texas have applications pending as of September 2024.
Unfortunately, it is unlkely that Canada would allow their prescription drugs to be shipped in large quantities to American consumers, not without imposing high tariffs as a disincentive. That is because drug manufacturers could limit supplies to Canada and cause shortages if drugs are moved to the U.S. Manufacturers could also be less willing to negotiate lower prices for Canadians if that will hurt U.S. profits.
Negotiating with the pharmaceutical industry
Be it prescription drugs or cars, both buyer and seller must agree on a price for a successful sale to occur. If the potential buyer is unwilling to walk away from negotiations, you will not get the seller’s best price. One reason U.S. drug prices are higher than other countries’ is because the government is not a shrewd negotiator.
Negotiations that result in major reductions in drug prices frequently result from the drug manufacturer losing access to patients on a certain health plan or ending up in a higher drug tier that substantially raises a patient’s copay. However, if the buyer refuses the seller’s final offer, their members or citizens lose access to those drugs. While major private health plans and pharmacy benefit managers are able to directly negotiate drug prices with pharmaceutical manufacturers, often with substantial savings, Medicare was prevented from doing so by federal law until recently.
In May 2018, the Trump administration released a so-called blueprint for reducing prescription drug prices that included negotiating Medicare prescription drug prices with the pharmaceutical industry. This plan wasn’t enacted during his term.
In August 2022, under the Biden-Harris administration, the Inflation Reduction Act enabled price negotiation and specified the number of drugs that negotiations could include in a year.

The first negotiation between Medicare and the pharmaceutical industry took place over the summer of 2024, lowering costs for 10 Medicare Part D drugs, which include the blood thinner Xarelto and the drugs Farxiga and Jardiance, which treat Type 2 diabetes, heart failure and kidney disease. The resulting $1.5 billion in savings will be extended in 2026 to the approximately 8.8 million Medicare Part D patients who are taking these drugs. The prices for these drugs are still twice what they are in four other developed countries.
Prices will be negotiated for another 15 Medicare Part D drugs in 2027. Thereafter, drug negotiations could include Medicare Part D drugs, which you pick up from your pharmacy, and Medicare Part B drugs, which are administered or received from your doctor’s office.
Another aspect of the Inflation Reduction Act is capping out-of-pocket expenses at $2,000. This won’t go into effect until 2025, however, and simply shifts costs above the cap onto taxpayers.
Continuation of progress
It is often challenging to attribute policy successes to one administration versus another when assessing complex issues such as drug pricing. There were ideas initiated during the Trump administration that did not come to fruition until the Biden-Harris administration implemented and expanded on them.
For example, Medicare price negotiation, proposed in a Trump administration “blueprint,” was codified in law by President Biden, but the fruits of this policy will not be seen until the next administration. And regardless of who you attribute this success to, only a portion of people on Medicare will see any relief from high drug prices as a result.
Truly lowering the costs of prescription drugs would require identifying the maximum price the nation is willing to pay for benefits, such as cost per quality adjusted life year at the federal, state and private payer levels, and being willing to walk away from negotiations if the price exceeds that level. This would not be a panacea, though, especially for patients with rare and ultrarare diseases, and would need to be eased in over time to avoid bankrupting the industry.![]()
C. Michael White, Distinguished Professor of Pharmacy Practice, University of Connecticut
This article is republished from The Conversation under a Creative Commons license. Read the original article.