News from the South - South Carolina News Feed
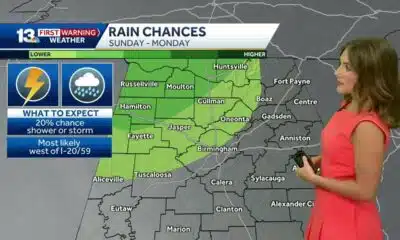
Cold Week Ahead
SUMMARY: December begins with chilly weather, characterized by dry conditions and a few flurries possible in the mountains. Average highs typically reach the upper 50s, but temperatures are expected to drop to the lower 50s and even 40s over the next several days. Western North Carolina might see afternoon highs in the 30s. A gradual warming trend is anticipated mid to late week, though cold and quiet conditions will prevail. Light snow is possible near the Tennessee-North Carolina border early next week. Overall, it’s essential to bundle up during this cold stretch as winter officially begins.
Cold temperatures this week
Subscribe to WYFF on YouTube now for more: http://bit.ly/1mUvbJX
Get more Greenville news: http://www.wyff4.com
Like us: http://www.facebook.com/WYFF4
Follow us: http://twitter.com/wyffnews4
Instagram: https://www.instagram.com/wyffnews4/
News from the South - South Carolina News Feed
Florence man sentenced to life in prison for killing girlfriend
SUMMARY: A Florence man, 50-year-old Derek Brunson, was sentenced to life in prison for the 2021 murder of his girlfriend, 31-year-old Caitlin Shipman, a mother of five. After a hung jury in his first trial, the second trial concluded in under an hour with a unanimous guilty verdict. Prosecutors described the killing as cold and methodical, highlighting Caitlin’s history of abuse and her coworkers’ testimonies about her fearful warnings. During sentencing, two of Caitlin’s children expressed relief that Brunson would be imprisoned for life. Family members hope this verdict brings justice and peace for Caitlin. Brunson’s defense claimed investigation flaws.
On Friday, Derrick Brunson was found guilty of murdering his girlfriend in May 2021 after a retrial. S.C. Circuit Court Judge Steven …
News from the South - South Carolina News Feed
High School football highlights: 9.12.25 (Part 1)
SUMMARY: The high school football highlights from Week 3 feature key matchups, including the undefeated Eastside Eagles’ 56-21 win over Blue Ridge, extending their nine-game winning streak against the Tigers. Westside started 0-2, losing 42-6 to unbeaten BHP Bears. Woodruff dominated Woodmont 48-6, while Powdersville won 35-7 at Pendleton, continuing their three-game streak. Dale Hannah secured a 40-27 victory over Wren. Byrnes defeated Greer 49-9, powered by Trey Segarra’s three touchdowns. Other notable results: Emerald beat Broome 42-18, Berea earned their first win vs. Southside, and Abbeville topped 96. A.C. Flora shut out Laurens 35-0. Coaches remain focused on improvement and upcoming region games.
High School football highlights: 9.12.25 (Part 1)
WYFF 4 is your home for South Carolina breaking news and weather. For your latest South Carolina news and weather visit: https://www.wyff4.com/
For licensing inquiries: https://www.wyff4.com/licensing
News from the South - South Carolina News Feed
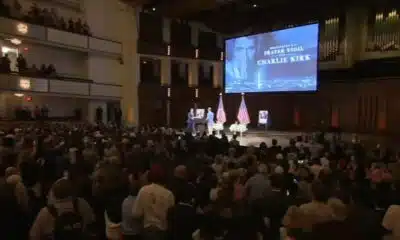
Suspect arrested, identified in shooting of Charlie Kirk, officials say
SUMMARY: A suspect, Tyler Robinson, has been arrested in the fatal shooting of conservative activist Charlie Kirk at Utah Valley University. Utah Gov. Spencer Cox confirmed the arrest, with President Trump also confirming custody and supporting the death penalty. Robinson’s father identified and convinced him to surrender. Authorities recovered a bolt-action rifle believed to be the murder weapon, with unusual cartridge markings under investigation. The shooting occurred from a rooftop during a public event, with Kirk killed by a single shot. Over 7,000 tips were received during the manhunt. Officials vow to hold the shooter accountable, calling it a “political assassination.”
The post Suspect arrested, identified in shooting of Charlie Kirk, officials say appeared first on www.abccolumbia.com
-
News from the South - Missouri News Feed7 days ago
1587 Prime gives first look at food, cocktail menu ahead of grand opening in KC
-
News from the South - West Virginia News Feed7 days ago
Protesters in D.C. flood the streets demanding an end to Trump’s military deployment
-
Mississippi News Video7 days ago
Interview: Come see Baptist at WTVA Senior Health Fair
-
News from the South - Arkansas News Feed6 days ago
‘One Pill Can Kill’ program aims to reduce opioid drug overdose
-
News from the South - Alabama News Feed6 days ago
Alabama lawmaker revives bill to allow chaplains in public schools
-
The Conversation7 days ago
How is paint made?
-
News from the South - Arkansas News Feed6 days ago
Arkansas’s morning headlines | Sept. 9, 2025
-
News from the South - Texas News Feed6 days ago
‘Resilience and hope’ in Galveston: 125 years after greatest storm in US history | Texas