Kaiser Health News
Amgen Plows Ahead With Costly, Highly Toxic Cancer Dosing Despite FDA Challenge

Arthur Allen
Tue, 07 May 2024 09:00:00 +0000
When doctors began using the drug sotorasib in 2021 with high expectations for its innovative approach to attacking lung cancer, retired medical technician Don Crosslin was an early beneficiary. Crosslin started the drug that July. His tumors shrank, then stabilized.
But while the drug has helped keep him alive, its side effects have gradually narrowed the confines of his life, said Crosslin, 76, who lives in Ocala, Florida: “My appetite has been minimal. I’m very weak. I walk my dogs and get around a bit, but I haven’t been able to golf since last July.”
He wonders whether he’d do better on a lower dose, “but I do what my oncologist tells me to do,” Crosslin said. Every day, he takes eight of the 120-milligram pills, sold under Amgen’s brand name Lumakras.
Crosslin’s concern lies at the heart of an FDA effort to make cancer drugs less toxic and more effective. Cancer drug trials are structured to promote high doses, which then become routine patient care. In the face of evidence that thousands of patients become so ill that they skip doses or stop taking the drugs — thereby risking resurgence of their cancers — the FDA has begun requiring companies to pinpoint the right dosage before they reach patients.
The initiative, Project Optimus, launched in 2021 just as Amgen was seeking to market sotorasib. At the time, the FDA’s leading cancer drug regulator, Richard Pazdur, co-authored an editorial in the New England Journal of Medicine that said Amgen’s trials of the $20,000-a-month drug were “hampered by a lack of robust dose exploration.”
The FDA conditionally approved sotorasib but required Amgen to conduct a study comparing the labeled dosage of 960 mg with a dosage of 240 mg. The trial, published in November, showed that the 960-mg dose may have given patients a month more of life, on average, but caused more severe side effects than the lower dose.
Amgen is keeping the 960-mg dosage as it conducts further tests to get final approval for the drug, spokesperson Elissa Snook said, adding that the dose showed superiority in one study. Whether medically justified or not, the heavier dosage allows the company to protect 75% of its revenue from the drug, which brought in nearly $200 million in the United States last year.
And there appears to be nothing the FDA can do about it.
“There’s a gap in FDA’s authority that results in patients getting excess doses of a drug at excess costs,” said Mark Ratain, a University of Chicago oncologist who has pushed for more accurate cancer drug dosing. “We should do something about this.”
Deciding on Dosage
It may be too late for the FDA to change the sotorasib dosage, although in principle it could demand a new regimen before granting final approval, perhaps in 2028. Under Project Optimus, however, the agency is doing something about dosage guidelines for future drugs. It is stressing dose optimization in its meetings with companies, particularly as they prepare to test drugs on patients for the first time, spokesperson Lauren-Jei McCarthy said.
“When you go in front of FDA with a plan to approve your drug now, they are going to address dosing studies,” said Julie Gralow, chief medical officer of the American Society of Clinical Oncology. “A lot of companies are struggling with this.”
That’s largely because the new requirements add six months to a year and millions in drug development costs, said Julie Bullock, a former FDA drug reviewer who advocated for more extensive dosing studies and is now senior vice president at Certara, a drug development consultancy.
In part, Project Optimus represents an effort to manage the faults of the FDA’s accelerated approval process, begun in 1992. While the process gets innovative drugs to patients more quickly, some medicines have proved lackluster or had unacceptable side effects.
That’s especially true of the newer pills to treat cancer, said Donald Harvey, an Emory University pharmacology professor, who has led or contributed to more than 100 early-phase cancer trials.
A study released last month in the Journal of the American Medical Association showed that 41% of the cancer drugs granted accelerated approval from 2013 to 2017 did not improve overall survival or quality of life after five years.
Many of these drugs flop because they must be given at toxic dosages to have any effect, Harvey said, adding that sotorasib might work better if the company had found an appropriate dosage earlier on.
“Sotorasib is a poster child for incredibly bad development,” Harvey said. The drug was the first to target the KRAS G12C mutation, which drives about 15% of lung cancers and was considered “undruggable” until University of California-San Francisco chemist Kevan Shokat figured out how to attack it in 2012.
Given the specificity of sotorasib’s target, Harvey said, Amgen could have found a lower dosage. “Instead, they followed the old model and said, ‘We’re going to push the dose up until we see a major side effect.’ They didn’t need to do that. They just needed more experience with a lower dose.”
The 960-mg dose “is really tough on patients,” said Yale University oncologist and assistant professor Michael Grant. “They get a lot of nausea and other GI side effects that are not pleasant. It hurts their quality of life.”
The FDA noted in its review of sotorasib that in phase 1 studies tumors shrank when exposed to as little as a fifth of the 960-mg daily dose Amgen selected. At all doses tested in that early trial, the drug reached roughly the same concentrations in the blood, which suggested that at higher doses the drug was mostly just intensifying side effects like diarrhea, vomiting, and mouth sores.
For most classes of drugs, companies spend considerable time in phases 1 and 2 of development, homing in on the right dosage. “No one would think of dosing a statin or antibiotic at the highest tolerable dose,” Ratain said.
Things are different in cancer drug creation, whose approach originated with chemotherapy, which damages as many cancer cells as possible, wrecking plenty of healthy tissue in the bargain. Typically, a company’s first series of cancer drug trials involve escalating doses in small groups of patients until something like a quarter of them get seriously ill. That “maximum tolerated dose” is then employed in more advanced clinical trials, and goes on the drug’s label. Once a drug is approved, a doctor can “go off-label” and alter the dosage, but most are leery of doing so.
Patients can find the experience rougher than advertised. During clinical trials, the side effects of the cancer drug osimertinib (Tagrisso) were listed as tolerable and manageable, said Jill Feldman, a lung cancer patient and advocate. “That killed me. After two months on that drug, I had lost 15 pounds, had sores in my mouth and down my throat, stomach stuff. It was horrible.”
Some practitioners, at least, have responded to the FDA’s cues on sotorasib. In the Kaiser Permanente health system, lung cancer specialists start with a lower dose of the drug, spokesperson Stephen Shivinsky said.
Smaller Doses — And Revenue
Amgen was clearly aware of the advantages of the 240-mg dosage before it sought FDA approval: It filed a provisional patent application on that dosage before the agency gave breakthrough approval for the drug at 960 mg. The company doesn’t appear to have disclosed the patent filing to investors or the FDA. McCarthy said the FDA was prohibited by law from discussing the particulars of its sotorasib regulation plans.
Switching to a 240-mg dosage could register a huge hit to Amgen’s revenue. The company markets the drug at more than $20,000 for a month of 960-mg daily doses. Each patient who could get by with a quarter of that would trim the company’s revenue by roughly $180,000 a year.
Amgen declined to comment on the patent issue or to make an official available to discuss the dosage and pricing issues.
Crosslin, who depends on Social Security for his income, couldn’t afford the $3,000 a month that Medicare required him to pay for sotorasib, but he has received assistance from Amgen and a charity that covers costs for patients below a certain income.
While the drug has worked well for Crosslin and other patients, its overall modest impact on lung cancer suggests that $5,000, rather than $20,000, might be a more appropriate price, Ratain said.
In the company’s phase 3 clinical trial for advanced lung cancer patients, sotorasib kept patients alive for about a month longer than docetaxel, the current, highly toxic standard of care. Docetaxel is a generic drug for which Medicare pays about $1 per injection. The trial was so unconvincing that the FDA sent Amgen back to do another.
Ratain, a staunch critic of Amgen’s handling of sotorasib, told Centers for Medicare & Medicaid Services officials at a recent meeting that they should pay for sotorasib on a basis of 240 mg per day. But CMS would do that only “if there is a change in the drug’s FDA-approved dosage,” spokesperson Aaron Smith said.
Drug companies generally don’t want to spend money on trials like the one the FDA ordered on sotorasib. In 2018, Ratain and other researchers used their institutions’ funding to conduct a dosing trial on the prostate cancer drug abiraterone, marketed under the brand name Zytiga by Johnson & Johnson. They found that taking one 250-mg pill with food was just as effective as taking four on an empty stomach, as the label called for.
Although J&J hasn’t changed the Zytiga label, the evidence generated in that trial was strong enough for the standards-setting National Comprehensive Cancer Network to change its recommendations.
Post-marketing studies like that one are hard to conduct, Emory’s Harvey said. Patients are reluctant to join a trial in which they may have to take a lower dosage, since most people tend to believe “the more the better,” he said.
“It’s better for everyone to find the right dose before a drug is out on the market,” Harvey said. “Better for the patient, and better for the company, which can sell more of a good drug if the patients aren’t getting sick and no longer taking it.”
——————————
By: Arthur Allen
Title: Amgen Plows Ahead With Costly, Highly Toxic Cancer Dosing Despite FDA Challenge
Sourced From: kffhealthnews.org/news/article/amgen-cancer-drug-sotorasib-lumakras-high-dosage-fda-dosing-trials/
Published Date: Tue, 07 May 2024 09:00:00 +0000
Kaiser Health News
US Judge Names Receiver To Take Over California Prisons’ Mental Health Program

SACRAMENTO, Calif. — A judge has initiated a federal court takeover of California’s troubled prison mental health system by naming the former head of the Federal Bureau of Prisons to serve as receiver, giving her four months to craft a plan to provide adequate care for tens of thousands of prisoners with serious mental illness.
Senior U.S. District Judge Kimberly Mueller issued her order March 19, identifying Colette Peters as the nominated receiver. Peters, who was Oregon’s first female corrections director and known as a reformer, ran the scandal-plagued federal prison system for 30 months until President Donald Trump took office in January. During her tenure, she closed a women’s prison in Dublin, east of Oakland, that had become known as the “rape club.”
Michael Bien, who represents prisoners with mental illness in the long-running prison lawsuit, said Peters is a good choice. Bien said Peters’ time in Oregon and Washington, D.C., showed that she “kind of buys into the fact that there are things we can do better in the American system.”
“We took strong objection to many things that happened under her tenure at the BOP, but I do think that this is a different job and she’s capable of doing it,” said Bien, whose firm also represents women who were housed at the shuttered federal women’s prison.
California corrections officials called Peters “highly qualified” in a statement, while Gov. Gavin Newsom’s office did not immediately comment. Mueller gave the parties until March 28 to show cause why Peters should not be appointed.
Peters is not talking to the media at this time, Bien said. The judge said Peters is to be paid $400,000 a year, prorated for the four-month period.
About 34,000 people incarcerated in California prisons have been diagnosed with serious mental illnesses, representing more than a third of California’s prison population, who face harm because of the state’s noncompliance, Mueller said.
Appointing a receiver is a rare step taken when federal judges feel they have exhausted other options. A receiver took control of Alabama’s correctional system in 1976, and they have otherwise been used to govern prisons and jails only about a dozen times, mostly to combat poor conditions caused by overcrowding. Attorneys representing inmates in Arizona have asked a judge to take over prison health care there.
Mueller’s appointment of a receiver comes nearly 20 years after a different federal judge seized control of California’s prison medical system and installed a receiver, currently J. Clark Kelso, with broad powers to hire, fire, and spend the state’s money.
California officials initially said in August that they would not oppose a receivership for the mental health program provided that the receiver was also Kelso, saying then that federal control “has successfully transformed medical care” in California prisons. But Kelso withdrew from consideration in September, as did two subsequent candidates. Kelso said he could not act “zealously and with fidelity as receiver in both cases.”
Both cases have been running for so long that they are now overseen by a second generation of judges. The original federal judges, in a legal battle that reached the U.S. Supreme Court, more than a decade ago forced California to significantly reduce prison crowding in a bid to improve medical and mental health care for incarcerated people.
State officials in court filings defended their improvements over the decades. Prisoners’ attorneys countered that treatment remains poor, as evidenced in part by the system’s record-high suicide rate, topping 31 suicides per 100,000 prisoners, nearly double that in federal prisons.
“More than a quarter of the 30 class-members who died by suicide in 2023 received inadequate care because of understaffing,” prisoners’ attorneys wrote in January, citing the prison system’s own analysis. One prisoner did not receive mental health appointments for seven months “before he hanged himself with a bedsheet.”
They argued that the November passage of a ballot measure increasing criminal penalties for some drug and theft crimes is likely to increase the prison population and worsen staffing shortages.
California officials argued in January that Mueller isn’t legally justified in appointing a receiver because “progress has been slow at times but it has not stalled.”
Mueller has countered that she had no choice but to appoint an outside professional to run the prisons’ mental health program, given officials’ intransigence even after she held top officials in contempt of court and levied fines topping $110 million in June. Those extreme actions, she said, only triggered more delays.
The 9th U.S. Circuit Court of Appeals on March 19 upheld Mueller’s contempt ruling but said she didn’t sufficiently justify calculating the fines by doubling the state’s monthly salary savings from understaffing prisons. It upheld the fines to the extent that they reflect the state’s actual salary savings but sent the case back to Mueller to justify any higher penalty.
Mueller had been set to begin additional civil contempt proceedings against state officials for their failure to meet two other court requirements: adequately staffing the prison system’s psychiatric inpatient program and improving suicide prevention measures. Those could bring additional fines topping tens of millions of dollars.
But she said her initial contempt order has not had the intended effect of compelling compliance. Mueller wrote as far back as July that additional contempt rulings would also be likely to be ineffective as state officials continued to appeal and seek delays, leading “to even more unending litigation, litigation, litigation.”
She went on to foreshadow her latest order naming a receiver in a preliminary order: “There is one step the court has taken great pains to avoid. But at this point,” Mueller wrote, “the court concludes the only way to achieve full compliance in this action is for the court to appoint its own receiver.”
This article was produced by KFF Health News, which publishes California Healthline, an editorially independent service of the California Health Care Foundation.
If you or someone you know may be experiencing a mental health crisis, contact the 988 Suicide & Crisis Lifeline by dialing or texting “988.”
The post US Judge Names Receiver To Take Over California Prisons’ Mental Health Program appeared first on kffhealthnews.org
Kaiser Health News
Amid Plummeting Diversity at Medical Schools, a Warning of DEI Crackdown’s ‘Chilling Effect’

The Trump administration’s crackdown on DEI programs could exacerbate an unexpectedly steep drop in diversity among medical school students, even in states like California, where public universities have been navigating bans on affirmative action for decades. Education and health experts warn that, ultimately, this could harm patient care.
Since taking office, President Donald Trump has issued a handful of executive orders aimed at terminating all diversity, equity, and inclusion, or DEI, initiatives in federally funded programs. And in his March 4 address to Congress, he described the Supreme Court’s 2023 decision banning the consideration of race in college and university admissions as “brave and very powerful.”
Last month, the Education Department’s Office for Civil Rights — which lost about 50% of its staff in mid-March — directed schools, including postsecondary institutions, to end race-based programs or risk losing federal funding. The “Dear Colleague” letter cited the Supreme Court’s decision.
Paulette Granberry Russell, president and CEO of the National Association of Diversity Officers in Higher Education, said that “every utterance of ‘diversity’ is now being viewed as a violation or considered unlawful or illegal.” Her organization filed a lawsuit challenging Trump’s anti-DEI executive orders.
While California and eight other states — Arizona, Florida, Idaho, Michigan, Nebraska, New Hampshire, Oklahoma, and Washington — had already implemented bans of varying degrees on race-based admissions policies well before the Supreme Court decision, schools bolstered diversity in their ranks with equity initiatives such as targeted scholarships, trainings, and recruitment programs.
But the court’s decision and the subsequent state-level backlash — 29 states have since introduced bills to curb diversity initiatives, according to data published by the Chronicle of Higher Education — have tamped down these efforts and led to the recent declines in diversity numbers, education experts said.
After the Supreme Court’s ruling, the numbers of Black and Hispanic medical school enrollees fell by double-digit percentages in the 2024-25 school year compared with the previous year, according to the Association of American Medical Colleges. Black enrollees declined 11.6%, while the number of new students of Hispanic origin fell 10.8%. The decline in enrollment of American Indian or Alaska Native students was even more dramatic, at 22.1%. New Native Hawaiian or other Pacific Islander enrollment declined 4.3%.
“We knew this would happen,” said Norma Poll-Hunter, AAMC’s senior director of workforce diversity. “But it was double digits — much larger than what we anticipated.”
The fear among educators is the numbers will decline even more under the new administration.
At the end of February, the Education Department launched an online portal encouraging people to “report illegal discriminatory practices at institutions of learning,” stating that students should have “learning free of divisive ideologies and indoctrination.” The agency later issued a “Frequently Asked Questions” document about its new policies, clarifying that it was acceptable to observe events like Black History Month but warning schools that they “must consider whether any school programming discourages members of all races from attending.”
“It definitely has a chilling effect,” Poll-Hunter said. “There is a lot of fear that could cause institutions to limit their efforts.”
Numerous requests for comment from medical schools about the impact of the anti-DEI actions went unreturned. University presidents are staying mum on the issue to protect their institutions, according to reporting from The New York Times.
Utibe Essien, a physician and UCLA assistant professor, said he has heard from some students who fear they won’t be considered for admission under the new policies. Essien, who co-authored a study on the effect of affirmative action bans on medical schools, also said students are worried medical schools will not be as supportive toward students of color as in the past.
“Both of these fears have the risk of limiting the options of schools folks apply to and potentially those who consider medicine as an option at all,” Essien said, adding that the “lawsuits around equity policies and just the climate of anti-diversity have brought institutions to this place where they feel uncomfortable.”
In early February, the Pacific Legal Foundation filed a lawsuit against the University of California-San Francisco’s Benioff Children’s Hospital Oakland over an internship program designed to introduce “underrepresented minority high school students to health professions.”
Attorney Andrew Quinio filed the suit, which argues that its plaintiff, a white teenager, was not accepted to the program after disclosing in an interview that she identified as white.
“From a legal standpoint, the issue that comes about from all this is: How do you choose diversity without running afoul of the Constitution?” Quinio said. “For those who want diversity as a goal, it cannot be a goal that is achieved with discrimination.”
UC Health spokesperson Heather Harper declined to comment on the suit on behalf of the hospital system.
Another lawsuit filed in February accuses the University of California of favoring Black and Latino students over Asian American and white applicants in its undergraduate admissions. Specifically, the complaint states that UC officials pushed campuses to use a “holistic” approach to admissions and “move away from objective criteria towards more subjective assessments of the overall appeal of individual candidates.”
The scrutiny of that approach to admissions could threaten diversity at the UC-Davis School of Medicine, which for years has employed a “race-neutral, holistic admissions model” that reportedly tripled enrollment of Black, Latino, and Native American students.
“How do you define diversity? Does it now include the way we consider how someone’s lived experience may be influenced by how they grew up? The type of school, the income of their family? All of those are diversity,” said Granberry Russell, of the National Association of Diversity Officers in Higher Education. “What might they view as an unlawful proxy for diversity equity and inclusion? That’s what we’re confronted with.”
California Attorney General Rob Bonta, a Democrat, recently joined other state attorneys general to issue guidance urging that schools continue their DEI programs despite the federal messaging, saying that legal precedent allows for the activities. California is also among several states suing the administration over its deep cuts to the Education Department.
If the recent decline in diversity among newly enrolled students holds or gets worse, it could have long-term consequences for patient care, academic experts said, pointing toward the vast racial disparities in health outcomes in the U.S., particularly for Black people.
A higher proportion of Black primary care doctors is associated with longer life expectancy and lower mortality rates among Black people, according to a 2023 study published by the JAMA Network.
Physicians of color are also more likely to build their careers in medically underserved communities, studies have shown, which is increasingly important as the AAMC projects a shortage of up to 40,400 primary care doctors by 2036.
“The physician shortage persists, and it’s dire in rural communities,” Poll-Hunter said. “We know that diversity efforts are really about improving access for everyone. More diversity leads to greater access to care — everyone is benefiting from it.”
This article was produced by KFF Health News, which publishes California Healthline, an editorially independent service of the California Health Care Foundation.
The post Amid Plummeting Diversity at Medical Schools, a Warning of DEI Crackdown’s ‘Chilling Effect’ appeared first on kffhealthnews.org
Kaiser Health News
Tribal Health Leaders Say Medicaid Cuts Would Decimate Health Programs

As Congress mulls potentially massive cuts to federal Medicaid funding, health centers that serve Native American communities, such as the Oneida Community Health Center near Green Bay, Wisconsin, are bracing for catastrophe.
That’s because more than 40% of the about 15,000 patients the center serves are enrolled in Medicaid. Cuts to the program would be detrimental to those patients and the facility, said Debra Danforth, the director of the Oneida Comprehensive Health Division and a citizen of the Oneida Nation.
“It would be a tremendous hit,” she said.
The facility provides a range of services to most of the Oneida Nation’s 17,000 people, including ambulatory care, internal medicine, family practice, and obstetrics. The tribe is one of two in Wisconsin that have an “open-door policy,” Danforth said, which means that the facility is open to members of any federally recognized tribe.
But Danforth and many other tribal health officials say Medicaid cuts would cause service reductions at health facilities that serve Native Americans.
Indian Country has a unique relationship to Medicaid, because the program helps tribes cover chronic funding shortfalls from the Indian Health Service, the federal agency responsible for providing health care to Native Americans.
Medicaid has accounted for about two-thirds of third-party revenue for tribal health providers, creating financial stability and helping facilities pay operational costs. More than a million Native Americans enrolled in Medicaid or the closely related Children’s Health Insurance Program also rely on the insurance to pay for care outside of tribal health facilities without going into significant medical debt. Tribal leaders are calling on Congress to exempt tribes from cuts and are preparing to fight to preserve their access.
“Medicaid is one of the ways in which the federal government meets its trust and treaty obligations to provide health care to us,” said Liz Malerba, director of policy and legislative affairs for the United South and Eastern Tribes Sovereignty Protection Fund, a nonprofit policy advocacy organization for 33 tribes spanning from Texas to Maine. Malerba is a citizen of the Mohegan Tribe.
“So we view any disruption or cut to Medicaid as an abrogation of that responsibility,” she said.
Tribes face an arduous task in providing care to a population that experiences severe health disparities, a high incidence of chronic illness, and, at least in western states, a life expectancy of 64 years — the lowest of any demographic group in the U.S. Yet, in recent years, some tribes have expanded access to care for their communities by adding health services and providers, enabled in part by Medicaid reimbursements.
During the last two fiscal years, five urban Indian organizations in Montana saw funding growth of nearly $3 million, said Lisa James, director of development for the Montana Consortium for Urban Indian Health, during a webinar in February organized by the Georgetown University Center for Children and Families and the National Council of Urban Indian Health.
The increased revenue was “instrumental,” James said, allowing clinics in the state to add services that previously had not been available unless referred out for, including behavioral health services. Clinics were also able to expand operating hours and staffing.
Montana’s five urban Indian clinics, in Missoula, Helena, Butte, Great Falls, and Billings, serve 30,000 people, including some who are not Native American or enrolled in a tribe. The clinics provide a wide range of services, including primary care, dental care, disease prevention, health education, and substance use prevention.
James said Medicaid cuts would require Montana’s urban Indian health organizations to cut services and limit their ability to address health disparities.
American Indian and Alaska Native people under age 65 are more likely to be uninsured than white people under 65, but 30% rely on Medicaid compared with 15% of their white counterparts, according to KFF data for 2017 to 2021. More than 40% of American Indian and Alaska Native children are enrolled in Medicaid or CHIP, which provides health insurance to kids whose families are not eligible for Medicaid. KFF is a health information nonprofit that includes KFF Health News.
A Georgetown Center for Children and Families report from January found the share of residents enrolled in Medicaid was higher in counties with a significant Native American presence. The proportion on Medicaid in small-town or rural counties that are mostly within tribal statistical areas, tribal subdivisions, reservations, and other Native-designated lands was 28.7%, compared with 22.7% in other small-town or rural counties. About 50% of children in those Native areas were enrolled in Medicaid.
The federal government has already exempted tribes from some of Trump’s executive orders. In late February, Department of Health and Human Services acting general counsel Sean Keveney clarified that tribal health programs would not be affected by an executive order that diversity, equity, and inclusion government programs be terminated, but that the Indian Health Service is expected to discontinue diversity and inclusion hiring efforts established under an Obama-era rule.
HHS Secretary Robert F. Kennedy Jr. also rescinded the layoffs of more than 900 IHS employees in February just hours after they’d received termination notices. During Kennedy’s Senate confirmation hearings, he said he would appoint a Native American as an assistant HHS secretary. The National Indian Health Board, a Washington, D.C.-based nonprofit that advocates for tribes, in December endorsed elevating the director of the Indian Health Service to assistant secretary of HHS.
Jessica Schubel, a senior health care official in Joe Biden’s White House, said exemptions won’t be enough.
“Just because Native Americans are exempt doesn’t mean that they won’t feel the impact of cuts that are made throughout the rest of the program,” she said.
State leaders are also calling for federal Medicaid spending to be spared because cuts to the program would shift costs onto their budgets. Without sustained federal funding, which can cover more than 70% of costs, state lawmakers face decisions such as whether to change eligibility requirements to slim Medicaid rolls, which could cause some Native Americans to lose their health coverage.
Tribal leaders noted that state governments do not have the same responsibility to them as the federal government, yet they face large variations in how they interact with Medicaid depending on their state programs.
President Donald Trump has made seemingly conflicting statements about Medicaid cuts, saying in an interview on Fox News in February that Medicaid and Medicare wouldn’t be touched. In a social media post the same week, Trump expressed strong support for a House budget resolution that would likely require Medicaid cuts.
The budget proposal, which the House approved in late February, requires lawmakers to cut spending to offset tax breaks. The House Committee on Energy and Commerce, which oversees spending on Medicaid and Medicare, is instructed to slash $880 billion over the next decade. The possibility of cuts to the program that, together with CHIP, provides insurance to 79 million people has drawn opposition from national and state organizations.
The federal government reimburses IHS and tribal health facilities 100% of billed costs for American Indian and Alaska Native patients, shielding state budgets from the costs.
Because Medicaid is already a stopgap fix for Native American health programs, tribal leaders said it won’t be a matter of replacing the money but operating with less.
“When you’re talking about somewhere between 30% to 60% of a facility’s budget is made up by Medicaid dollars, that’s a very difficult hole to try and backfill,” said Winn Davis, congressional relations director for the National Indian Health Board.
Congress isn’t required to consult tribes during the budget process, Davis added. Only after changes are made by the Centers for Medicare & Medicaid Services and state agencies are tribes able to engage with them on implementation.
The amount the federal government spends funding the Native American health system is a much smaller portion of its budget than Medicaid. The IHS projected billing Medicaid about $1.3 billion this fiscal year, which represents less than half of 1% of overall federal spending on Medicaid.
“We are saving more lives,” Malerba said of the additional services Medicaid covers in tribal health care. “It brings us closer to a level of 21st century care that we should all have access to but don’t always.”
This article was published with the support of the Journalism & Women Symposium (JAWS) Health Journalism Fellowship, assisted by grants from The Commonwealth Fund.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
The post Tribal Health Leaders Say Medicaid Cuts Would Decimate Health Programs appeared first on kffhealthnews.org
-

 Mississippi Today6 days ago
Mississippi Today6 days agoLawmakers used to fail passing a budget over policy disagreement. This year, they failed over childish bickering.
-

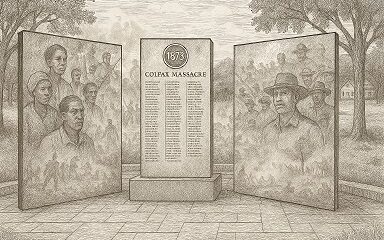
 Mississippi Today6 days ago
Mississippi Today6 days agoOn this day in 1873, La. courthouse scene of racial carnage
-

 Local News7 days ago
Local News7 days agoAG Fitch and Children’s Advocacy Centers of Mississippi Announce Statewide Protocol for Child Abuse Response
-

 Local News6 days ago
Local News6 days agoSouthern Miss Professor Inducted into U.S. Hydrographer Hall of Fame
-

 News from the South - Alabama News Feed4 days ago
News from the South - Alabama News Feed4 days agoFoley man wins Race to the Finish as Kyle Larson gets first win of 2025 Xfinity Series at Bristol
-

 News from the South - Alabama News Feed5 days ago
News from the South - Alabama News Feed5 days agoFederal appeals court upholds ruling against Alabama panhandling laws
-

 News from the South - Florida News Feed7 days ago
News from the South - Florida News Feed7 days agoSevere weather has come and gone for Central Florida, but the rain went with it
-

 News from the South - Alabama News Feed6 days ago
News from the South - Alabama News Feed6 days agoBellingrath Gardens previews its first Chinese Lantern Festival