Matthew Hill/Bloomberg Creative Photos via Getty Images
Daniel Freedman, University of Wisconsin-Stout
The colors of rubies and emeralds are so striking that they define shades of red and green – ruby red and emerald green. But have you ever wondered how they get those colors?
I am an inorganic chemist. Researchers in my field work to understand the chemistry of all the elements that make up the periodic table. Many inorganic chemists focus on the transition metals – the elements in the middle of the periodic table. The transition metals include most of the metals you are familiar with, like iron (Fe) and gold (Au).
One feature of compounds made with transition metals is their intense color. There are many examples in nature, including gemstones and paint pigments. Even the color of blood comes from the protein hemoglobin, which contains iron.
Investigating the colors of compounds containing transition metals leads you into some really amazing science – that’s part of what drew me to study this field.
Rubies and emeralds are great examples of how a small amount of a transition metal – in this case, chromium – can create a beautiful color in what would otherwise be a fairly boring-looking mineral.
Minerals and crystals

benedek/E+ via Getty Images
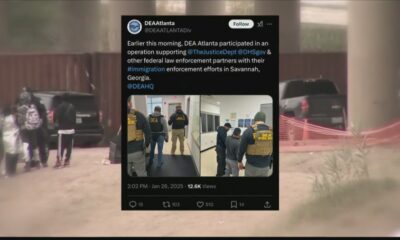
Both rubies and emeralds are minerals, which is a type of rock with a consistent chemical composition and a highly ordered structure at the atomic level.
When this highly ordered structure extends in all three dimensions, the mineral becomes a crystal.
With a theory developed by physicists in the 1920s called crystal field theory, scientists can explain why rubies and emeralds have the colors they do. Crystal field theory makes predictions about how a transition metal ion’s structure is affected by the other atoms surrounding it.
Rubies are mainly made up of the mineral corundum, which is composed of the elements aluminum and oxygen in a regular, repeating array. Each aluminum ion is surrounded by six oxygen ions.
Eigenes Werk/Wikimedia Commons, CC BY-SA
Emeralds are mainly made up of the mineral beryl, which is made from the elements beryllium, aluminum, silicon and oxygen. Beryl’s crystal structure is more complicated than corundum’s because of the additional elements in the formula, but each aluminum ion is again surrounded by six oxygen ions.

SunChan/E+ via Getty Images
Pure corundum and beryl are colorless. The brilliant colors of rubies and emeralds come from the presence of very small amounts of chromium. The chromium replaces about 1% of the aluminum in the corundum or beryl crystal when a ruby or emerald forms underground at a high temperature and pressure.
But how can one element – chromium – create the red color of a ruby and green color of an emerald?
Color science
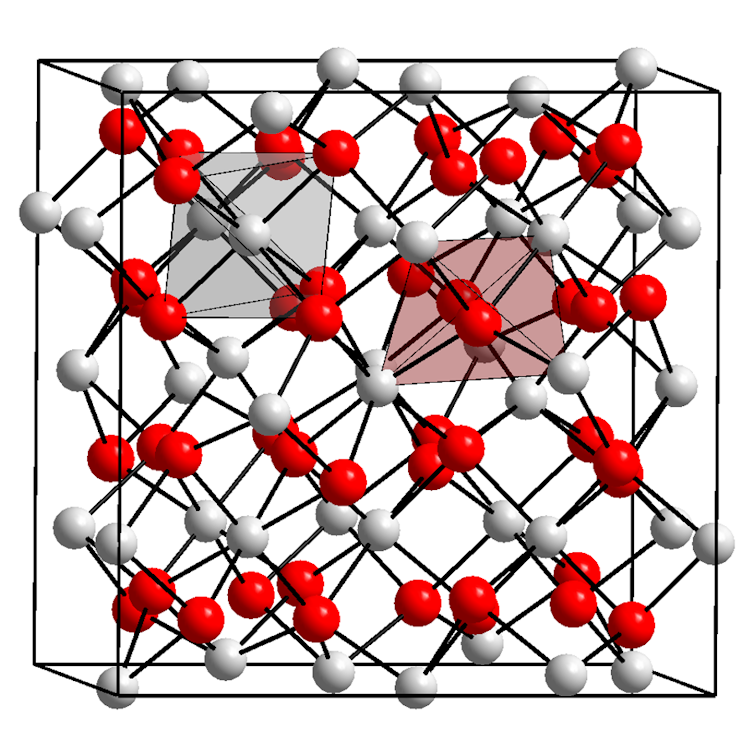
Rubies and emeralds have the colors they do because, like many substances, they absorb some colors of light. Most visible light, like sunlight, is composed of all the colors of the rainbow: red, orange, yellow, green, blue, indigo and violet. These colors make up the visible light spectrum, which is easy to remember as ROY G BIV.
Fulvio314/Wikimedia Commons, CC BY-SA
One of the main reasons why objects have a color is because they absorb one or more of these visible colors of light. If a substance absorbs, for instance, red light, it means that the red light gets trapped in the substance and the other colors reflect back to your eyes. The color you see is the sum of the remaining light, which will be in the green-to-blue range. If a substance absorbs blue, it will look red or orange to you.
Unlike the colorless aluminum ion, the chromium ion absorbs blue and green light when surrounded by the oxygen ions. The red light is reflected back, so that’s what you see in rubies.
In an emerald, even though the chromium is surrounded by six oxygen ions, there is a weaker interaction between the chromium and the surrounding oxygen ions. That’s due to the presence of silicon and beryllium in the beryl crystal. They cause the emerald to absorb blue and red light, leaving the green for you to see.
The ability to tune the properties of transition metals like chromium through changing what is surrounding it is a core strategy in my field of inorganic chemistry. Doing so can help scientists understand the basic science of metal-containing compounds and the design of chemical compounds for specific purposes.
You can take delight in the amazing colors of the gemstones, but through chemistry, you can also see how nature creates those colors using an endless variety of complex structures made with the elements in the periodic table.![]()
Daniel Freedman, Dean of the College of Science, Technology, Engineering, Mathematics & Management, University of Wisconsin-Stout
This article is republished from The Conversation under a Creative Commons license. Read the original article.