News from the South - North Carolina News Feed
A choking death, an abusive resident, missed medications, and a 0-star rating, state records show • Asheville Watchdog
A Woodfin assisted living facility failed to call 911 for a resident who choked twice and subsequently died, did not supervise or discharge an aggressive resident who physically assaulted other residents and staff for more than two months, and administered medications late or not at all, state inspection records show.
Harmony at Reynolds Mountain has a rating of zero stars out of four from state regulators. The facility previously had a three-star rating.
The severity of the violations in 2024 led regulators to suspend admissions for more than three months and impose fines of $33,000; Harmony has appealed $21,000 of the penalties.
In a response to questions from Asheville Watchdog, Harmony said in a statement it “is proud of the tremendous progress the community has made following staffing challenges that are common in the industry and reviews of our operations that highlighted opportunities for improvement.”
The “assertions” in the inspections “have been fully addressed and resolved,” the statement said, and the facility “has undergone significant changes, including the installation of a stable and experienced leadership team.” Some of the deficiencies “date back as long as a year ago,” a spokesman said.
“A recent survey by state regulators highlighted substantial improvements, with compliance noted across key areas and overwhelmingly positive feedback from residents and their families,” Harmony’s statement said.
In September, the state informed Harmony it intended to downgrade the facility’s license to provisional but in early December dropped that and lifted the suspension of admissions, citing “progress towards substantial compliance” with regulations.
The North Carolina Department of Health and Human Services visited the 99-bed facility three times in 2024 for inspections and in response to complaints. Records from those inspections show:
– Harmony failed to administer medications as prescribed to residents with conditions including diabetes, high blood pressure, and Parkinson’s disease, in some cases resulting in worsened symptoms. Reasons included “waiting on pharmacy,” “med not available,” and “med not in cart.”
– Top positions at the facility frequently turned over or were vacant. The administrator as of April was also in the same role at a “sister facility” in another state and had not visited Harmony in seven months.
– In interviews with inspectors, an aide said, “We do not have enough staff by any stretch of the imagination,” and a resident said she had recently waited an hour for assistance getting off the toilet.
Harmony did not answer questions from The Watchdog about its star rating, turnover and whether it was a practice at other Harmony sites for the administrator to be located in another state.
In response to the inspections, Harmony outlined measures to correct violations that included training and oversight over the administration of medications and staffing and the use of contract labor to cover shortages.
How to check out an ALF
Visit the state’s licensure page and search by county or facility name. Click on the facility to view inspection reports, star ratings and penalties.
Harmony was cited for three of the most serious violations – those that result in death, serious harm or neglect – over the care of the resident who choked, turned blue, and lost consciousness in July. State records do not name the resident, but The Watchdog identified her through public records as Christa Koppe.
Harmony administrators did not call 911 when Koppe choked, as the inspection report said their policy mandated, nor did they inform her family, her son, Oliver, said.
Two days after Koppe choked, a physician making rounds in the facility ordered her diet changed to pureed food, but staff failed to carry out the order, records show. Koppe choked the following day after receiving a regular diet meal, and again Harmony failed to call 911.
Koppe died that night from hypoxia, or low oxygen levels, and asphyxiation pneumonia, complications of choking and inhaling food or liquids into the lungs.
“Wow, that’s shocking,” Oliver Koppe told The Watchdog. “They just called that evening and said that she choked and passed away.”
At the time, Koppe said, he was surprised. His mother, who was 84 and had dementia, “was pretty stout, able to walk, did everything fine,” he said. “She just couldn’t remember things, but she was very capable.”
Koppe, who is a nurse, said he now believes his mother’s death may have been preventable.
“It was just so egregious,” Oliver’s wife, Carrie, said after reading the state’s inspection report. “There were so many points they could have made the right decision. They didn’t follow their own policy.”
Harmony did not respond to specific questions about its treatment of Koppe and notifications to her family.
In response to the state’s findings, Harmony increased oversight and trained staff on responding to emergencies and ensuring dietary orders are followed, according to a Plan of Correction.
‘I thought she was getting top quality care’
Three Asheville area families who entrusted Harmony with their loved ones told The Watchdog they chose the facility because it was newly built, clean, and promised premium care.
Harmony charged $5,200 to $8,400 a month for an apartment in assisted living, depending on the size, and another $600 to $2,400 monthly for care, depending on the level required, according to a recent price sheet provided by a family member.
“We went with them because they were a real nice facility and expensive,” Oliver Koppe said. “I thought she was getting top quality care.”
Harmony charged $9,200 a month for Koppe’s memory care, her daughter-in-law said.
Opened in 2016 and originally called The Crossings at Reynolds Mountain, Harmony is a “senior living community offering independent living, assisted living, and secured memory care,” with apartments, garden patios, restaurant-style dining, and social events, according to its website.
The Asheville location is one of 45 in 12 states run by the family-owned Harmony Senior Services, started by James R. Smith, who is also founder of Smith/Packett of Roanoke, a senior housing developer.
Harmony was “founded on the belief that people deserve higher quality senior living options,” the company’s website says. “It is an honor for our family to provide each resident, family member, and associate with the same care, compassion, and respect we would our own family.”
Debra Walker liked that Harmony was close to her north Asheville home and she could check each day on her mother, who was in memory care from August 2020 through December 2022.
But after observing what she described as inconsistent care and insufficient staffing, Walker said, she often visited two to three times a day to ensure her mother was clean, ate and stayed hydrated.
“If I was going to be out of town, I would have people go in and check on her,” Walker said. “There were some truly wonderful [staff] there, but it took a heroic effort for them to do their job.”
Harmony charged $8,122 a month for her mother’s memory care plus another $500 for “extensive incontinence” care and $500 for meal assistance, which Walker said involved cutting up her food.
Billie Marzullo bought a home near Harmony while the facility was under construction. Her husband, Larry, who had Parkinson’s disease, lived at Harmony on three occasions.
“We were thrilled to think that there would be a high-quality, progressive care facility within blocks of our front door,” she said.
But Marzullo said she became dissatisfied with persistent staffing shortages and her husband’s care.

Marzullo said she drew a clock for staff to show the importance of adhering to a schedule for his medications. With no improvement, she moved him in June 2023 to an assisted living facility in Colorado that she said was superior to Harmony.
From 2018 through 2022, Harmony received a 3-star rating from the state Division of Health Service Regulation’s adult care licensure section, which regulates homes and assisted living facilities for people who need help with daily activities. Nursing homes provide chronic or rehabilitative care and fall under a different regulatory section, while independent living is not regulated.

Stars are based on scores from inspections. Facilities must obtain two consecutive annual inspection scores of 100 or higher for four stars; three stars is 90 or higher, two stars, 80 to 89.9, and so on. Zero stars means a score below 70.
Fifty-four of the 63 licensed adult care homes and facilities in Buncombe have three or four stars. Of the five with zero stars, Harmony had the lowest score as of December, which was -0.5, according to the state’s website.
The Watchdog submitted questions to the state health and human services department, including whether inspectors attributed the violations found at Harmony to persistent staff shortages and turnover at the top. “A number of factors may impact a facility’s compliance, including management,” a spokeswoman responded via email.
State law allows the department to revoke a facility’s license when it fails to comply with regulations and “it is not reasonably probable” the deficiencies will be corrected in a reasonable time period or the facility will remain in compliance. Violations endangering “the health, safety, or welfare of the patients” can also be cause for revocation.
Based on an analysis of the law, the department “did not revoke the license of Harmony” and declined to downgrade its license to provisional “since the facility remedied the most serious licensure violations as determined on the follow-up survey” on Nov. 8, the spokeswoman said.
Hitting, biting, choking: Aggressive resident unsupervised
Inspectors from the state and Buncombe County’s Department of Social Services visited Harmony last year in April for an annual survey and complaint investigation. Their report said:
A resident with dementia and depression had become increasingly aggressive beginning in December 2023, when she punched another resident in the face. By March, she had struck three more residents, two on the head, and threatened another with a raised fist.
Aides described to inspectors multiple incidences of aggression by the resident. One said she observed her shoving and pinning another resident to the floor.
Another said the resident “hit, slapped, and choked staff,” and had bitten a resident.
Staff were trained to “just do the best we can” and “keep their distance,” one of the aides said.
Harmony sent the resident to the emergency room after three incidents, but the hospital “kept sending her back to the facility without treatment,” the health and wellness director told inspectors.
Notes from a contracted mental health provider in January 2024 said the resident had “slapped multiple staff members…We may need to consider transferring this resident to a different facility.” A February note from the provider said the resident was hitting and biting other residents and “required a one-on-one sitter for her own safety and the safety of other residents.”
The resident’s “responsible party,” typically a family member, “decided not to procure a sitter,” the inspection report said. She told inspectors she refused “because she thought her behaviors were medication induced” but agreed to a sitter about a month later following another assault, the report said.
To protect residents, staff began locking their rooms; residents could exit on their own but needed assistance to re-enter.
Harmony’s administrator told inspectors the aggressive resident “should have been required to have a sitter” and that “locking resident doors was not an appropriate safety plan in response to resident aggression.”

The interim executive director told inspectors he thought the resident had a sitter earlier. “It was an oversight that no other protective action had been taken,” the director said.
Harmony failed to discharge the resident as required when other residents were endangered, inspectors found. Discharge decisions were up to the health and wellness director, who told inspectors in February “she had not considered initiating a discharge yet because she had not thought about it.”
Regulators cited Harmony with violations for failing to supervise the aggressive resident or initiate her discharge and for not protecting the other residents. The administrator “failed to ensure responsibility for the operations of the facility,” resulting in “resident rights being violated,” the inspection report states.
Administrators and staff at Harmony were not identified by name in the reports.
In response to the findings, Harmony’s regional operations specialist trained all managers on “how to ensure residents were protected by providing supervision, maintaining their resident rights and how to appropriately discharge a resident who was mentally and physically abusive,” according to a Plan of Correction.
Residents behaving aggressively would be sent to the hospital and evaluated to determine if they are “appropriate to return,” the plan said. Harmony said it would immediately discharge residents when the well-being of others was jeopardized and “ensure one-on-one supervision until discharge.”
‘Delay of care’ after choking
Inspectors returned to Harmony in August to follow up and in response to two complaints from the county’s social services department. Their report details Koppe’s choking episodes and the failure by administrators to seek medical attention for her. (Koppe is listed in the report as Resident #1; The Watchdog is substituting her name for clarity.)
Koppe choked during lunch on July 9, “turned blue and lost consciousness,” according to the report. Two hospice nursing assistants, who were visiting Harmony and heard staff yelling, performed the Heimlich maneuver and cleared Koppe’s airway.

A Harmony aide assigned to monitor the residents during lunch “did not know what to do,” according to the report. “He was trained on the Heimlich Maneuver, but he had not performed it on a real person before.”
One of the hospice aides said she asked an administrator if Koppe would be sent to the hospital and was told no, because the resident choked “quite a bit.”
Harmony’s policy requires calling 911 when a resident chokes or loses consciousness. The resident care director said she checked on Koppe about 15 minutes after she choked and that “with her experience, she knew [Koppe] was fine.”
On July 11, a doctor making rounds at Harmony ordered a chest X-ray “for evaluation of possible aspiration pneumonia,” the report said. Koppe’s diet was also changed from soft food to pureed.
But on July 12, she received a “regular diet” at breakfast “and started having some heavy coughing episodes and choked,” a medication aide told inspectors. Koppe also received a regular lunch, but the aide removed it “once she noticed it,” the report said.
About 90 minutes after lunch, Koppe began “coughing very bad and vomiting a lot,” the aide told inspectors. The aide said she asked the resident care director (RCD) “at what point did she need to send [Koppe] to the hospital for evaluation and was told by the RCD that she thought [Koppe] had aspiration pneumonia and as long as the phlegm was coming out then [Koppe] was ‘ok.’ ”
That evening, an aide entered Koppe’s room to administer bedtime medications and found her unresponsive, with vomit on her clothes.
It was only then that the facility called 911. By the time paramedics arrived, Koppe was dead.
Koppe’s primary care doctor told inspectors she should have been medically evaluated immediately after the first choking episode, especially with her history of esophageal cancer. She said Koppe was “at a very high risk for complications,” including “hypoxia related to aspiration.”
Koppe died from hypoxia with aspiration pneumonia as a contributing cause, according to her death certificate.
State regulators cited Harmony with failing to ensure Koppe’s dietary orders were followed and not contacting 911 or her doctor when she choked, resulting “in a delay of care and treatment” that led to her death.
In response, a nurse consultant and clinical specialist trained all Harmony associates on CPR, “responding to an emergency, providing assistance to residents, and calling 911,” according to a Plan of Correction. Staff were also trained in reporting and documenting a change in condition, including choking episodes.
Dietary staff were trained on managing diet orders, which were also audited for accuracy. The executive director or designee would review diet orders monthly or upon a change in condition, and staff would ensure food trays were consistent with diet orders, the plan said.
Missed medications, doctors’ orders not followed
During inspections in April, August, November and January, state regulators documented medication problems at Harmony, including failure to administer drugs as prescribed, state records show.
Medications were improperly administered to 5 of 13 residents reviewed in the August inspection.
A drug used to treat symptoms of Parkinson’s disease such as tremors and stiffness was supposed to be administered within an hour of the prescribed time, the inspection report said.
For one resident, the drug was given outside that one-hour window on 46 of 91 occasions in July.
A mental health provider under contract to Harmony told inspectors the drug “must be taken at the same time every day to prevent ‘wearing off’” of such symptoms as difficulty walking or standing and muscle rigidity. Inconsistent administration of the drug, the provider said, “could cause very painful and debilitating symptoms.”

A medication aide told inspectors she was aware she administered the drug “late on multiple occasions” but said “there were not enough staff to assist with medication administration.”
For another resident with diabetes, a doctor ordered blood sugar checks with a finger stick three times a day, but records showed multiple missed tests for reasons including “waiting on glucose strips,” “no glucose strips on the cart” and “refused.” In July alone, the facility failed to obtain blood sugar checks on the resident a quarter of the time.
Harmony failed to administer a medication for a resident’s high blood pressure as prescribed, ”which resulted in her lower extremities swelling and weeping and increased her risk of developing congestive heart failure,” inspectors wrote.
Another resident with diabetes was supposed to receive a prescribed drug daily unless the resident’s blood sugar was less than 200. Records showed the resident’s blood sugar was below that threshold nearly every day from late June through mid August, but the medication was still given at least 14 times.
A medication aide told inspectors “she did not realize she had given the medication when it was to be held because she was not paying attention to the parameters.”
The doctor for a resident with heart failure instructed Harmony to notify her of weight changes of more than three pounds, a sign of worsening health that could require hospitalization. Records showed the resident’s weight fluctuated as much as 35.7 pounds from June through August, but the doctor was never notified.
Staff failed to measure daily weights of another resident with congestive heart failure about half the time. A medication aide told inspectors she was aware she should have informed the doctor but “did not have time. She had to administer medications to residents on two separate floors.”
The resident care director, who had been on the job about two months, told inspectors “she was still learning her responsibilities, and putting out all the ‘fires.’”
Harmony’s administrator, who had been on the job a week, blamed “lack of training and accountability.”
Inspectors in August cited Harmony with failing to administer medications as ordered and within an hour of the prescribed time.
Harmony trained staff on reporting and documenting any change of condition and missed or refused medications, according to a Plan of Correction. The facility initiated an order tracking system at each nurse’s station and said it would run a “missed medication report” daily, med cart audits weekly and “a time variance report no less than weekly.” Vital sign reports would be reviewed monthly.
Inspectors returned in November and found a more serious medication violation corrected but cited Harmony for not administering medications as ordered.
Two residents went without anti-anxiety drugs, one for 19 days, “increasing the risk of anxiety, agitation, and aggression,” according to the November inspection report.
Harmony also failed to administer pain, blood pressure, and other medications within an hour of the prescribed times to two residents reviewed.
One resident told inspectors his morning medications were often late and that “staff were ‘stretched thin.’” Aides could not tell him what medications they were administering, the resident said, and “he had no way of knowing if he got the correct medications or not.”
An aide acknowledged to inspectors “she could not always administer medications within the scheduled time frame” and said she had “been working short staffed” and dispensing medications to residents on two floors for two months since another aide quit.
Harmony’s executive director, who had been on the job about a week, told inspectors she was not aware the resident’s medications were late. ”The facility was short-staffed and hired agency staff to cover shifts,” she said.
Harmony conducted audits and trained staff on “medication reordering policies to ensure medications/supplies are available and followed per MD order,” according to a November Plan of Protection.
Inspectors visited Harmony in mid-January and found the facility had failed to administer a vitamin supplement to a resident on multiple days because it was not in the medication cart. The administrator told inspectors she did not know why the medication aides had not notified the pharmacy and that “a pharmacy consultant recently conducted an audit and did not find any issues.”
The January inspection found Harmony remained out of compliance on medication administration but at a level no longer considered a violation, a state DHHS spokeswoman said.
Staff shortages from top to bottom
Harmony had at least three executive directors in 2024, records show. The administrator as of April told inspectors that she had been on the job since January, “after the previous Administrator abruptly resigned.”
She was the administrator of “a sister facility” and did not even live in North Carolina. She told inspectors that she had last been to Harmony in August 2023, seven months earlier.
The report did not give a reason for the previous administrator’s resignation, and Harmony did not respond to a question seeking an explanation.
The administrator “entrusted the operations of the facility” to the interim executive director who along with the health and wellness director were responsible for managing resident care, she told inspectors. “There had been some turnover” in both of those positions, she said.
The administrator said she had “had only two conversations” with the executive director in the six weeks since he started.

The health care director position was vacant, and a mental health provider told inspectors in March, “There had been a lot of turnover at the facility.”
Vacancies extended to the staff assigned to directly care for residents. Inspectors found Harmony failed to meet minimum staff requirements on three shifts during a two-week period in July.
In interviews with inspectors in August:
– The resident who said she had to wait an hour for assistance getting off the toilet also told inspectors “staff routinely told her when they responded to her call light that they only had one staff member assigned to provide care for all the residents who lived on the first, second, and third floors.” At that time, 60 residents lived on those three floors, the inspection report said.
– A personal care aide said “residents would at times get tired of waiting for staff to come help them and they would try to get up without assistance,” increasing their risk of falls.
– A medication aide said “there had recently been a lot of falls. . . We do not have enough staff by any stretch of the imagination.”
Harmony had brought in staff from temporary agencies, and the health and wellness director told inspectors “they were actively recruiting new staff at the local community college and at job fairs.”

A complaint investigation by county social services workers in August found delays in responding to residents’ calls for assistance. During a three-day period reviewed, it took staff 20 minutes to 67 minutes to answer one resident’s calls.
The resident said she “wets herself regularly while waiting for assistance to use the bathroom” and had learned to “ ‘convince’ herself” that she didn’t need to go “because she knows staff won’t come in time.”
An aide told inspectors, “Resident showers were getting missed because some residents needed two person assists and they didn’t have enough staff.”
Harmony did not have a policy on response time for residents’ calls, but the administrator told inspectors staff were trained to respond within five minutes and “it should not take longer than 20 minutes.”
In response to the inspections, Harmony said it had contracts with labor agencies to cover shortages and would conduct weekly audits to ensure compliance with staffing requirements. The clinical specialist “educated staff to ensure there is coverage in [sic] building before they leave.”
During the November visit, inspectors found that a resident who was incontinent went seven hours without care. All residents were supposed to be checked at least every two hours, the executive director told inspectors.
The resident was “at high risk for skin breakdown due to incontinence and mobility issues,” the inspection report said. A personal care aide told inspectors he was the only one on duty that shift covering three floors.
The health and wellness director pitched in but told inspectors she “was only answering residents that used their call lights to request assistance.” The executive director told inspectors she was aware of “some staffing challenges” that day but had been assured “everything was being covered.”
A Plan of Protection following the November inspection said that “interviewable residents” were interviewed and “stated their needs were met.” It also said education would be provided to clinical teams on two-hour checks of residents.
State takes action, notes improvements
On Aug. 21, state regulators suspended admissions at Harmony.
“The documented violations indicate that conditions in the home are found to be detrimental to the health and safety of the residents,” said a letter from the chief of adult care licensure. “Therefore, it is the finding of this agency that the facility has failed to provide services to assure the health, safety, and welfare of the residents.”
On Sept. 12, the state informed Harmony that based upon the violations found in April and August, “the Department intends to downgrade your license to provisional,” a probation-type status that requires corrections be made within three months and follow-up visits by regulators. A facility’s license to operate can be suspended or revoked if it fails to comply.

During the November visit, state inspectors found the most serious violations at Harmony had been corrected, and on Dec. 5, the state lifted its suspension of admissions and said it no longer intended to downgrade Harmony’s license to provisional.
“We find Harmony at Reynolds Mountain has made progress towards substantial compliance with the rules for the licensing of Adult Care Homes,” the licensure chief wrote in a letter to the facility’s executive director.
Harmony has appealed three of the fines imposed by the state following the April inspection and totaling $21,000. The other, for $12,000, is due, according to the Department of Health and Human Services.
Additional “penalties have been recommended and are being processed” for the violations found in August, a DHHS spokeswoman said.
Harmony did not respond to specific questions about the inspection findings.
The company instead pointed to its response after Tropical Storm Helene on Sept. 27, saying in its statement that Harmony “distinguished itself as a beacon of resilience and care,” maintaining uninterrupted meal service and medication access, delivering essential supplies, and securing water and fuel.
Harmony “today is a community on an upward trajectory, supported by strong leadership, dedicated staff, and a shared commitment to excellence,” the statement said. “While we have had operational challenges in the past, as have all senior living facilities and healthcare providers, they do not define who we are or where we are heading.
“Harmony remains focused on providing a safe, warm, and supportive environment for the older adults who choose to call Reynolds Mountain their home.”
Asheville Watchdog is a nonprofit news team producing stories that matter to Asheville and Buncombe County. Sally Kestin is a Pulitzer Prize-winning investigative reporter. Email skestin@avlwatchdog.org. The Watchdog’s reporting is made possible by donations from the community. To show your support for this vital public service go to avlwatchdog.org/support-our-publication/.
Related
The post A choking death, an abusive resident, missed medications, and a 0-star rating, state records show • Asheville Watchdog appeared first on avlwatchdog.org
News from the South - North Carolina News Feed
Bipartisan bill in Congress would fund repairs to private roads damaged by Hurricane Helene • NC Newsline
SUMMARY: A bipartisan group of North Carolina lawmakers introduced the “Restoring Access to Mountain Homes Act,” aimed at securing federal reimbursements for repairing private infrastructure damaged by Hurricane Helene. The bill would allow state, local, and tribal governments to receive funds for restoring over 8,000 private roads and bridges, which are crucial for rural residents’ access to emergency services and daily necessities. U.S. Rep. Chuck Edwards emphasized the unprecedented damage caused by the hurricane. The bill requires damage inspections and adherence to FEMA’s documentation rules to ensure timely recovery for the affected communities in western North Carolina.
The post Bipartisan bill in Congress would fund repairs to private roads damaged by Hurricane Helene • NC Newsline appeared first on ncnewsline.com
News from the South - North Carolina News Feed
Jones: Hurricane recovery biggest sham ever on North Carolina taxpayers | North Carolina
SUMMARY: Republican Rep. Brendan Jones criticized the North Carolina Office of Resiliency and Recovery, calling its slow progress on post-hurricane rebuilding a “sham” to taxpayers. He expressed frustration over persistent delays in completing recovery projects for families impacted by Hurricanes Matthew and Florence, with many still waiting for assistance. The office’s interim head, Pryor Gibson, acknowledged the challenges and thanked the legislature for an $80 million appropriation. While Gibson hopes for completion in the east this year, Jones urged for quicker action. Additionally, Jones drew comparisons to “Groundhog Day” and expressed concerns about the state’s management of recovery efforts.
The post Jones: Hurricane recovery biggest sham ever on North Carolina taxpayers | North Carolina appeared first on www.thecentersquare.com
News from the South - North Carolina News Feed
Mission Health in Western NC faces renewed scrutiny after Helene
Instrumental in Helene aftermath, Mission Health ‘back to their old ways’
Asheville’s Mission Health has been trying to help the city recover in the aftermath of Tropical Storm Helene. But medical staff and state officials have not softened their stance toward the beleaguered hospital.
New North Carolina Attorney General Jeff Jackson, for one, is not backing down from his office’s lawsuit against the medical provider.
The lawsuit, originally filed in 2023 by predecessor Josh Stein, who is now the governor, accuses parent company HCA Healthcare of reneging on a promise to maintain oncology and emergency services. Stein also claims that the hospital is guilty of understaffing, long wait times and bed shortages.
“I know HCA was hopeful that a new attorney general would drop our office’s lawsuit,” Jackson told Carolina Public Press. “I am the attorney general, and that’s not going to happen.
“HCA broke the promises it made to provide emergency and cancer-care services to the people of Western North Carolina. We’ll keep fighting for this case as long as it takes to restore the health care HCA promised to provide and Western North Carolinians deserve.”
Mission Health’s Helene help
Meanwhile, Mission Health is still trying to recover after Helene left the facility without water for more than two months. Staff, many of whom suffered losses from the storm themselves, worked for days at a time to deal with an influx of storm-related injuries and illnesses.
Pop-up stores were created so they could grab essential supplies.
Stations were set up where they could shower and do laundry.
Gas tanks were filled for free.
By many accounts, Mission Health cared for their employees in the immediate aftermath of the storm.
But that was then.
Now, some hospital staff feel that HCA Healthcare, and Mission Health by extension, has returned to its “old ways.”
“We are right back to cutting corners and making money off of understaffing,” said Kerri Wilson, a Mission Health nurse. “I would say the safety and staffing issues within the hospital are pretty reflective of the way they were in late 2023 when we were placed in ‘immediate jeopardy.’ If surveyors came by over this past weekend, I feel we could go back into ‘immediate jeopardy’ very easily.”
Double ‘jeopardy’
“Immediate Jeopardy” is the most serious citation that the Centers for Medicaid and Medicare can deliver to a hospital. And, like Wilson referenced, that’s what happened in December 2023 when the organization notified HCA Healthcare that Mission Health had been cited for nine instances of patient harm or avoidable deaths in 2022 and 2023.
“The ER is almost full every day, the ICU has been full, so we’ve had patients waiting for extended periods of time,” Wilson explained. “There were reports of nurses having to take care of up to 12 patients each.”
The most common recommendation for nurse-to-patient ratios is one nurse for every four patients.
“There were a few good things that happened after the hurricane,” Wilson continued. “We were able to get gas tanks and things like that during those first, really tough weeks of healing. But as soon as the cameras and the media and FEMA started to leave the area, we saw that a lot of those good things stopped. HCA was putting on a show. It was a lot of PR stunts for them, and that was really disappointing because I gave them the benefit of the doubt.
“They are back to their old ways, and our patients are suffering because of it.”
View from the top
But HCA Healthcare’s top leader holds a different view.
CEO Greg Lowe argues that HCA Healthcare’s status as the largest hospital corporation in the country is what allowed them to serve patients through Helene.
“Because of the support from HCA Healthcare, Mission Hospital and our five acute-care community hospitals were able to remain open to care for our neighbors throughout the storm and its devastating aftermath,” Lowe said in a statement. “Thinking about how we have been able to consistently serve our communities … makes me incredibly grateful to be part of this team. Without HCA Healthcare’s scale and ability to deliver under immense pressure, Mission Health facilities would have been otherwise forced to close.”
Even the hospital’s harshest critics partially agree with that assessment. Julie Mayfield, a Democratic state senator who represents Buncombe County, is one of them. Mayfield heads a coalition of physicians, nurses, elected officials, business leaders, clergy and advocates whose mission is to replace HCA Healthcare as owner of Mission Health with a nonprofit hospital system.
“They really took care of their employees and patients in a way that was kind of surprising to everyone,” Mayfield told CPP. “They would never have been able to do everything they did, as quickly, if they weren’t a major corporation. What the storm showed us, very clearly, is that they have the resources and can make the investments in their patients and employees if it is in their interest.
“But we’re a little bit past that now, and we’re starting to hear some problematic and troubling things from folks on the inside again. They didn’t just wake up and become the company we want them to be.”
Mission Health monopoly
Not only did Stein sue Mission Health for cutting services in Asheville, he’s also been outspoken about what he sees as a health care monopoly in the region.
When a need was found for a hospital in the Buncombe County town of Weaverville, Stein urged North Carolina’s Department of Health Human Services to deny Mission Health’s application.
“Currently, Mission has almost no competition for acute care in Buncombe County. The lack of competition is the result of Mission’s unique history,” he wrote.
The department ultimately awarded the right to build a facility to AdventHealth, a Florida company that operates hospitals in Polk and Henderson counties as well as eight other states.
But the deal isn’t done yet.
On Jan. 13, HCA once again appealed the state’s decision, sending the issue back to court and further delaying the construction of the Weaverville facility.
“We strongly believe Mission Hospital can best meet Western North Carolina’s growing need for complex medical and surgical care,” HCA spokeswoman Nancy Lindell told CPP. “If we had been awarded the beds, Mission Hospital could have had these beds available in the shortest period of time — beds which are desperately needed by our community.”
This article first appeared on Carolina Public Press and is republished here under a Creative Commons license.![]()
-

 News from the South - North Carolina News Feed6 days ago
News from the South - North Carolina News Feed6 days agoTrump International Airport proposed, renaming Dulles | North Carolina
-

 News from the South - Kentucky News Feed6 days ago
News from the South - Kentucky News Feed6 days agoTrump’s new Justice Department leadership orders a freeze on civil rights cases
-
 News from the South - Kentucky News Feed6 days ago
News from the South - Kentucky News Feed6 days agoThawing out from the deep freeze this weekend
-

 Mississippi News Video7 days ago
Mississippi News Video7 days ago1/23/25- The “freezer door” shuts after Saturday AM, then the warm up begins!
-

 News from the South - Florida News Feed5 days ago
News from the South - Florida News Feed5 days agoDemocrats and voting groups say a bid to toss out North Carolina ballots is an attack on democracy
-

 News from the South - Missouri News Feed7 days ago
News from the South - Missouri News Feed7 days agoMissouri Republicans plan to challenge abortion initiative this session
-
 News from the South - Louisiana News Feed6 days ago
News from the South - Louisiana News Feed6 days agoCauseway reopens to drivers in Louisiana
-
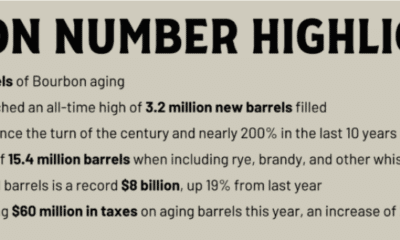
 News from the South - Kentucky News Feed3 days ago
News from the South - Kentucky News Feed3 days agoKentucky’s bourbon industry worries as potential 50% EU-imposed tariffs loom