Kaiser Health News
Why Long-Term Care Insurance Falls Short for So Many
Jordan Rau, KFF Health News and JoNel Aleccia, KFF Health News
Wed, 22 Nov 2023 10:00:00 +0000
For 35 years, Angela Jemmott and her five brothers paid premiums on a long-term care insurance policy for their 91-year-old mother. But the policy does not cover home health aides whose assistance allows her to stay in her Sacramento, California, bungalow, near the friends and neighbors she loves. Her family pays $4,000 a month for that.
“We want her to stay in her house,” Jemmott said. “That’s what’s probably keeping her alive, because she’s in her element, not in a strange place.”
The private insurance market has proved wildly inadequate in providing financial security for most of the millions of older Americans who might need home health aides, assisted living, or other types of assistance with daily living.
For decades, the industry severely underestimated how many policyholders would use their coverage, how long they would live, and how much their care would cost.
And as Jemmott belatedly discovered, the older generation of plans — those from the 1980s — often covered only nursing homes.
Only 3% to 4% of Americans 50 and older pay for a long-term care policy, according to LIMRA, an insurance marketing and research association. That stands in stark contrast to federal estimates that 70% of people 65 and older will need critical services before they die.
Repeated government efforts to create a functioning market for long-term care insurance — or to provide public alternatives — have never taken hold. Today, most insurers have stopped selling stand-alone long-term care policies: The ones that still exist are too expensive for most people. And they have become less affordable each year, with insurers raising premiums higher and higher. Many policyholders face painful choices to pay more, pare benefits, or drop coverage altogether.
“It’s a giant bait-and-switch,” said Laura Lunceford, 69, of Sandy, Utah, whose annual premium with her husband leaped to more than $5,700 in 2019 from less than $3,800. Her stomach knots up a couple of months before the next premium is due, as she fears another spike. “They had a business model that just wasn’t sustainable from the get-go,” she said. “Why they didn’t know that is beyond me, but now we’re getting punished for their lack of foresight.”
The glaring gaps in access to coverage persist despite steady increases in overall payouts. Last year, insurers paid more than $13 billion to cover 345,000 long-term care claims, according to industry figures. Many policyholders and their relatives reported that their plans helped them avert financial catastrophes when they faced long-term care costs that would have otherwise eviscerated their savings.
But others have been startled to learn that policies they paid into over decades will not fully cover the escalating present-day costs of home health aides, assisted living facilities, or nursing homes. And in other cases, people entitled to benefits confront lengthy response times to coverage requests or outright denials, according to records kept by the National Association of Insurance Commissioners, the organization of state regulators.
Jesse Slome, executive director of the American Association for Long-Term Care Insurance, an industry trade group, said long-term care was the most challenging type of insurance to manage. “You need multiple crystal balls,” Slome said. “And you have to look 20 years into the future and be right.”
The Pandemic Paused a Long-Term Decline
The industry’s wobbly finances haven’t steadied despite a brief profitable surge during the coronavirus pandemic. Earnings rose because thousands of people who were drawing benefits, many in nursing homes or assisted living facilities, died from covid-19, and other policyholders died before using their insurance. Others stopped tapping their benefits because they fled facilities and went to live with their families, who provided unpaid care.
Overall, earnings went from $2.3 billion in losses in 2019 to two years of profits totaling $1.1 billion, before receding into the red in 2022 by losing $304 million, according to Fitch Ratings.
Still, none of that was enough to reverse the industry’s long-term decline. Doug Baker, a director in Fitch’s U.S. life insurance group, said long-term care insurance “is one of the riskiest in our universe” because of the lingering financial burden from underestimating the number of people who would tap their policies.
More insurers now offer hybrid plans that combine life insurance with long-term care. Those policies are less generous than the ones offered a decade ago — and using the long-term care benefit drains some or all of the money policyholders hoped to leave to their heirs.
“I don’t think people will offer unlimited again,” said Tom McInerney, the chief executive of Genworth Financial, which suspended selling plans through brokers in 2019. “One way or another, taxpayers are going to have to pay more for long-term care needs of the baby boomers.”
Many experts believe it’s untenable to expect that a private insurance market can protect most people from the growing burden of long-term care costs.
“The whole situation is poorly suited to that kind of insurance offering,” said Robert Saldin, a political science professor at the University of Montana who studies the industry.
Falling Profits and Skyrocketing Premiums
Starting in the 1970s, long-term care insurance was touted as a way to keep older people from eroding their retirement savings or resorting to Medicaid, the state-federal program for the poor and disabled. Early plans were limited to nursing home care but later expanded to cover in-home care and assisted living centers. Sales of the policies doubled from 1990 to 2002.
As demand grew, however, there were signs the industry had vastly miscalculated the cost of its products. Insurers set early policy prices competitively low, based on actuarial models that turned out to be markedly inaccurate. Forecasters’ estimates of policyholders’ longevity were wrong. U.S. life expectancy increased to nearly 77 years in 2000 from about 68 years in 1950, federal records show. And as people lived longer, their need for care increased.
Industry officials also failed to account for the behavior of savvy consumers determined to keep their long-term care coverage. Insurers counted on policy lapse rates — people giving up their policies or defaulting on payments — of about 4% annually. The actual lapse rate was closer to 1%.
As the miscalculations sent profits plummeting, insurers raised premiums or exited the market. By 2020, sales of traditional policies had dropped to 49,000 and the number of carriers offering plans had fallen to fewer than a dozen from more than 100.
Premiums for some consumers doubled in just a year or two. Three class-action lawsuits accused Genworth of failing to disclose to policyholders that it had planned multiyear rate increases, leaving them without information they needed to decide whether to keep their policies. Genworth settled the lawsuits with offers to allow customers to adjust their policies, and in some cases it paid cash damage to those who accepted reduced benefits. The company did not admit wrongdoing.
The increases continue. AM Best, a rating agency, said in a report last November that Genworth “will continue to need annual rate increases for at least several more years to reach economic break-even.”
Prices for new policies have jumped, too. A decade ago, a couple aged 55 could expect to pay about $3,725 a year for a policy that included $162,000 in total benefits and 3% annual inflation protection, according to the American Association for Long-Term Care Insurance. Today, a policy that is virtually the same would cost $5,025, 35% more, even as rising health costs and inflation have eroded the value of the benefits.
And that’s only for the people who can qualify. To limit their losses, insurers have narrowed the eligible pool of clients. In 2021, about 30% of applicants ages 60 to 64 were denied long-term care insurance. For applicants 70 to 74, the rejection rate was 47%. Even among people in their 50s, more than 1 in 5 were turned down. Chronic health conditions, a history of stroke or diabetes, or psychiatric illness may all be grounds for disqualification.
At the same time, insurers began scrutinizing claims more closely. “They tightened their belts,” said Alan Kassan, a senior partner with the California law firm Kantor & Kantor, which represents clients challenging denials. “Then they tightened their claim administration and started denying claims more and more.”
In 2022, the proportion of traditional long-term care claim denials varied, from 4.5% in Rhode Island to 9.6% in Alaska, according to the National Association of Insurance Commissioners.
Despite efforts to limit liability, financial problems forced several high-profile insurance providers to drastically revise policy terms and premiums or go into insolvency, affecting the investments of thousands of clients.
They included Alice Kempski, a retired nurse who, after her husband died, bought a policy from the insurance company Penn Treaty and American Network in 2004 on the advice of a financial adviser, paying premiums of $180 a month for 16 years. By 2017, she was hobbled by osteoporosis and was struggling to manage her multiple medications, according to her daughter, Ann Kempski. She sold the family home in Wilmington, Delaware, in 2017 and, now needing help bathing, moved to an assisted living center there. But when the family tried to file a claim, they discovered that Penn Treaty was insolvent and the policy had been taken over by the Pennsylvania state insurance guaranty fund.
The fund had frozen Kempski’s benefits and increased her premiums to about $280 a month, her daughter said. Her doctor told Penn that she had “mild dementia” and osteoporosis and should be in an assisted living facility. But the insurer said that there was not enough evidence that she needed help with two daily living activities or had severe cognitive impairment, conditions that would trigger coverage, according to correspondence between Kempski and the company.
Kempski was paying roughly $5,400 a month out-of-pocket to the assisted living center. She moved in with her daughter when the pandemic hit, but she continued to pay full rent to the facility to save her spot until she returned in 2021. In March of that year, when her daughter was preparing to refile a claim for long-term care insurance and her premiums had reached $320 a month, Kempski had a massive stroke. She died the next month. The insurer never paid for any of her care.
Coverage in a Facility but Not at Home
The policy held by Angela Jemmott’s mother, Jewell Thomas, went unused for a different reason: Like many older policies, it covered only skilled nursing care in a facility. Her children had purchased the policy after Thomas’ husband died at 56.
But decades later, once Thomas developed dementia in her 80s, her children realized how desperately their mother wanted to stay home. Jemmott said they tried to add a rider to the policy to cover home care but were told that their mother’s age (older than 75) barred add-ons. Now the siblings jointly pay about $4,000 a month for two home health aides, while still paying the insurance premium of more than $2,500 a year. “We feel like if we stop paying it, another unforeseen need will arise and cause us to wish we kept it,” Jemmott said.
Not all policyholders are displeased.
Bert Minushkin, of Royal Palm Beach, Florida, paid monthly premiums for 27 years, beginning in 1993 when the policy was offered as a benefit by Westinghouse Electric Corp., where he worked as a nuclear engineer. Over time, he paid about $120,000 toward the policy, said his daughter Lisa Heffley, 61, of Louisville, Kentucky.
Diagnosed with dementia, Minushkin began declining swiftly in 2019. His wife spent $220,000 on assisted living facilities and private aides for him over three years, with about $90,000 of the cost offset by his policy, Heffley said. He died in February 2022 at age 91.
“He didn’t break even, but thank God he had it,” she said.
Turning to Crowdfunding
Many experts say what’s needed is a government-subsidized or public program that requires people to carry long-term care insurance, as the Netherlands and Singapore have. But federal efforts to create such a system, including the CLASS Act, which was repealed in 2013, and the WISH Act, introduced in 2021, have failed to gain traction in Congress. At the state level, Washington this summer started a first-in-the-nation program that will provide long-term care benefits for residents who pay into a fund, but it is voluntary, and the maximum benefit of $36,500 will not cover a year in most assisted living facilities.
Lack of a safety net leaves some people unprotected, like Jeffrey Tanck, a real estate broker in Washington, D.C. In 2021, his mother, Sue Tanck, at 75, suffered a serious fall, leaving her with broken arms and a traumatic brain injury. She had been the primary caretaker for his father, Roger, then 77, who had rapidly worsening dementia.
Without warning, Jeffrey Tanck had to assume charge of his father’s care, moving him into an assisted living center in Ocala, Florida, that now charges $4,600 a month, and had to get his mother into a skilled nursing facility paid for by Medicaid. With no money to cover his father’s costs until he sold their house, Tanck resorted to a plea on the crowdfunding site GoFundMe.
Wanting to shield himself from a similar financial crisis somewhere down the road, Tanck, who is 51, applied for long-term care insurance, only to be denied. The reason? He takes antidepressants, which help him cope with the anxiety and stress of caring for his parents.
“What are people supposed to do?” Tanck asked. “I’m going to need something.”
——————————
By: Jordan Rau, KFF Health News and JoNel Aleccia, KFF Health News
Title: Why Long-Term Care Insurance Falls Short for So Many
Sourced From: kffhealthnews.org/news/article/dying-broke-why-long-term-care-insurance-falls-short/
Published Date: Wed, 22 Nov 2023 10:00:00 +0000
Did you miss our previous article…
https://www.biloxinewsevents.com/from-hospital-to-hospitality-spin-doctors-brand-getting-sick-as-an-adventure-its-not/
Kaiser Health News
States Brace for Reversal of Obamacare Coverage Gains Under Trump’s Budget Bill
Shorter enrollment periods. More paperwork. Higher premiums. The sweeping tax and spending bill pushed by President Donald Trump includes provisions that would not only reshape people’s experience with the Affordable Care Act but, according to some policy analysts, also sharply undermine the gains in health insurance coverage associated with it.
The moves affect consumers and have particular resonance for the 19 states (plus Washington, D.C.) that run their own ACA exchanges.
Many of those states fear that the additional red tape — especially requirements that would end automatic reenrollment — would have an outsize impact on their policyholders. That’s because a greater percentage of people in those states use those rollovers versus shopping around each year, which is more commonly done by people in states that use the federal healthcare.gov marketplace.
“The federal marketplace always had a message of, ‘Come back in and shop,’ while the state-based markets, on average, have a message of, ‘Hey, here’s what you’re going to have next year, here’s what it will cost; if you like it, you don’t have to do anything,’” said Ellen Montz, who oversaw the federal ACA marketplace under the Biden administration as deputy administrator and director at the Center for Consumer Information and Insurance Oversight. She is now a managing director with the Manatt Health consulting group.
Millions — perhaps up to half of enrollees in some states — may lose or drop coverage as a result of that and other changes in the legislation combined with a new rule from the Trump administration and the likely expiration at year’s end of enhanced premium subsidies put in place during the covid-19 pandemic. Without an extension of those subsidies, which have been an important driver of Obamacare enrollment in recent years, premiums are expected to rise 75% on average next year. That’s starting to happen already, based on some early state rate requests for next year, which are hitting double digits.
“We estimate a minimum 30% enrollment loss, and, in the worst-case scenario, a 50% loss,” said Devon Trolley, executive director of Pennie, the ACA marketplace in Pennsylvania, which had 496,661 enrollees this year, a record.
Drops of that magnitude nationally, coupled with the expected loss of Medicaid coverage for millions more people under the legislation Trump calls the “One Big Beautiful Bill,” could undo inroads made in the nation’s uninsured rate, which dropped by about half from the time most of the ACA’s provisions went into effect in 2014, when it hovered around 14% to 15% of the population, to just over 8%, according to the most recent data.
Premiums would rise along with the uninsured rate, because older or sicker policyholders are more likely to try to jump enrollment hurdles, while those who rarely use coverage — and are thus less expensive — would not.
After a dramatic all-night session, House Republicans passed the bill, meeting the president’s July 4 deadline. Trump is expected to sign the measure on Independence Day. It would increase the federal deficit by trillions of dollars and cut spending on a variety of programs, including Medicaid and nutrition assistance, to partly offset the cost of extending tax cuts put in place during the first Trump administration.
The administration and its supporters say the GOP-backed changes to the ACA are needed to combat fraud. Democrats and ACA supporters see this effort as the latest in a long history of Republican efforts to weaken or repeal Obamacare. Among other things, the legislation would end several changes put in place by the Biden administration that were credited with making it easier to sign up, such as lengthening the annual open enrollment period and launching a special program for very low-income people that essentially allows them to sign up year-round.
In addition, automatic reenrollment, used by more than 10 million people for 2025 ACA coverage, would end in the 2028 sign-up season. Instead, consumers would have to update their information, starting in August each year, before the close of open enrollment, which would end Dec. 15, a month earlier than currently.
That’s a key change to combat rising enrollment fraud, said Brian Blase, president of the conservative Paragon Health Institute, because it gets at what he calls the Biden era’s “lax verification requirements.”
He blames automatic reenrollment, coupled with the availability of zero-premium plans for people with lower incomes that qualify them for large subsidies, for a sharp uptick in complaints from insurers, consumers, and brokers about fraudulent enrollments in 2023 and 2024. Those complaints centered on consumers’ being enrolled in an ACA plan, or switched from one to another, without authorization, often by commission-seeking brokers.
In testimony to Congress on June 25, Blase wrote that “this simple step will close a massive loophole and significantly reduce improper enrollment and spending.”
States that run their own marketplaces, however, saw few, if any, such problems, which were confined mainly to the 31 states using the federal healthcare.gov.
The state-run marketplaces credit their additional security measures and tighter control over broker access than healthcare.gov for the relative lack of problems.
“If you look at California and the other states that have expanded their Medicaid programs, you don’t see that kind of fraud problem,” said Jessica Altman, executive director of Covered California, the state’s Obamacare marketplace. “I don’t have a single case of a consumer calling Covered California saying, ‘I was enrolled without consent.’”
Such rollovers are common with other forms of health insurance, such as job-based coverage.
“By requiring everyone to come back in and provide additional information, and the fact that they can’t get a tax credit until they take this step, it is essentially making marketplace coverage the most difficult coverage to enroll in,” said Trolley at Pennie, 65% of whose policyholders were automatically reenrolled this year, according to KFF data. KFF is a health information nonprofit that includes KFF Health News.
Federal data shows about 22% of federal sign-ups in 2024 were automatic-reenrollments, versus 58% in state-based plans. Besides Pennsylvania, the states that saw such sign-ups for more than 60% of enrollees include California, New York, Georgia, New Jersey, and Virginia, according to KFF.
States do check income and other eligibility information for all enrollees — including those being automatically renewed, those signing up for the first time, and those enrolling outside the normal open enrollment period because they’ve experienced a loss of coverage or other life event or meet the rules for the low-income enrollment period.
“We have access to many data sources on the back end that we ping, to make sure nothing has changed. Most people sail through and are able to stay covered without taking any proactive step,” Altman said.
If flagged for mismatched data, applicants are asked for additional information. Under current law, “we have 90 days for them to have a tax credit while they submit paperwork,” Altman said.
That would change under the tax and spending plan before Congress, ending presumptive eligibility while a person submits the information.
A white paper written for Capital Policy Analytics, a Washington-based consultancy that specializes in economic analysis, concluded there appears to be little upside to the changes.
While “tighter verification can curb improper enrollments,” the additional paperwork, along with the expiration of higher premiums from the enhanced tax subsidies, “would push four to six million eligible people out of Marketplace plans, trading limited fraud savings for a surge in uninsurance,” wrote free market economists Ike Brannon and Anthony LoSasso.
“Insurers would be left with a smaller, sicker risk pool and heightened pricing uncertainty, making further premium increases and selective market exits [by insurers] likely,” they wrote.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
This article first appeared on KFF Health News and is republished here under a Creative Commons license.
The post States Brace for Reversal of Obamacare Coverage Gains Under Trump’s Budget Bill appeared first on kffhealthnews.org
Note: The following A.I. based commentary is not part of the original article, reproduced above, but is offered in the hopes that it will promote greater media literacy and critical thinking, by making any potential bias more visible to the reader –Staff Editor.
Political Bias Rating: Center-Left
This content presents a critique of Republican-led changes to the Affordable Care Act, emphasizing potential negative impacts such as increased premiums, reduced enrollment, and the erosion of coverage gains made under the ACA. It highlights the perspective of policy analysts and state officials who express concern over these measures, while also presenting conservative viewpoints, particularly those focusing on fraud reduction. Overall, the tone and framing lean toward protecting the ACA and its expansions, which traditionally aligns with Center-Left media analysis.
Kaiser Health News
Dual Threats From Trump and GOP Imperil Nursing Homes and Their Foreign-Born Workers
In a top-rated nursing home in Alexandria, Virginia, the Rev. Donald Goodness is cared for by nurses and aides from various parts of Africa. One of them, Jackline Conteh, a naturalized citizen and nurse assistant from Sierra Leone, bathes and helps dress him most days and vigilantly intercepts any meal headed his way that contains gluten, as Goodness has celiac disease.
“We are full of people who come from other countries,” Goodness, 92, said about Goodwin House Alexandria’s staff. Without them, the retired Episcopal priest said, “I would be, and my building would be, desolate.”
The long-term health care industry is facing a double whammy from President Donald Trump’s crackdown on immigrants and the GOP’s proposals to reduce Medicaid spending. The industry is highly dependent on foreign workers: More than 800,000 immigrants and naturalized citizens comprise 28% of direct care employees at home care agencies, nursing homes, assisted living facilities, and other long-term care companies.
But in January, the Trump administration rescinded former President Joe Biden’s 2021 policy that protected health care facilities from Immigration and Customs Enforcement raids. The administration’s broad immigration crackdown threatens to drastically reduce the number of current and future workers for the industry. “People may be here on a green card, and they are afraid ICE is going to show up,” said Katie Smith Sloan, president of LeadingAge, an association of nonprofits that care for older adults.
Existing staffing shortages and quality-of-care problems would be compounded by other policies pushed by Trump and the Republican-led Congress, according to nursing home officials, resident advocates, and academic experts. Federal spending cuts under negotiation may strip nursing homes of some of their largest revenue sources by limiting ways states leverage Medicaid money and making it harder for new nursing home residents to retroactively qualify for Medicaid. Care for 6 in 10 residents is paid for by Medicaid, the state-federal health program for poor or disabled Americans.
“We are facing the collision of two policies here that could further erode staffing in nursing homes and present health outcome challenges,” said Eric Roberts, an associate professor of internal medicine at the University of Pennsylvania.
The industry hasn’t recovered from covid-19, which killed more than 200,000 long-term care facility residents and workers and led to massive staff attrition and turnover. Nursing homes have struggled to replace licensed nurses, who can find better-paying jobs at hospitals and doctors’ offices, as well as nursing assistants, who can earn more working at big-box stores or fast-food joints. Quality issues that preceded the pandemic have expanded: The percentage of nursing homes that federal health inspectors cited for putting residents in jeopardy of immediate harm or death has risen alarmingly from 17% in 2015 to 28% in 2024.
In addition to seeking to reduce Medicaid spending, congressional Republicans have proposed shelving the biggest nursing home reform in decades: a Biden-era rule mandating minimum staffing levels that would require most of the nation’s nearly 15,000 nursing homes to hire more workers.
The long-term care industry expects demand for direct care workers to burgeon with an influx of aging baby boomers needing professional care. The Census Bureau has projected the number of people 65 and older would grow from 63 million this year to 82 million in 2050.
In an email, Vianca Rodriguez Feliciano, a spokesperson for the Department of Health and Human Services, said the agency “is committed to supporting a strong, stable long-term care workforce” and “continues to work with states and providers to ensure quality care for older adults and individuals with disabilities.” In a separate email, Tricia McLaughlin, a Department of Homeland Security spokesperson, said foreigners wanting to work as caregivers “need to do that by coming here the legal way” but did not address the effect on the long-term care workforce of deportations of classes of authorized immigrants.
Goodwin Living, a faith-based nonprofit, runs three retirement communities in northern Virginia for people who live independently, need a little assistance each day, have memory issues, or require the availability of around-the-clock nurses. It also operates a retirement community in Washington, D.C. Medicare rates Goodwin House Alexandria as one of the best-staffed nursing homes in the country. Forty percent of the organization’s 1,450 employees are foreign-born and are either seeking citizenship or are already naturalized, according to Lindsay Hutter, a Goodwin spokesperson.
“As an employer, we see they stay on with us, they have longer tenure, they are more committed to the organization,” said Rob Liebreich, Goodwin’s president and CEO.
Jackline Conteh spent much of her youth shuttling between Sierra Leone, Liberia, and Ghana to avoid wars and tribal conflicts. Her mother was killed by a stray bullet in her home country of Liberia, Conteh said. “She was sitting outside,” Conteh, 56, recalled in an interview.
Conteh was working as a nurse in a hospital in Sierra Leone in 2009 when she learned of a lottery for visas to come to the United States. She won, though she couldn’t afford to bring her husband and two children along at the time. After she got a nursing assistant certification, Goodwin hired her in 2012.
Conteh said taking care of elders is embedded in the culture of African families. When she was 9, she helped feed and dress her grandmother, a job that rotated among her and her sisters. She washed her father when he was dying of prostate cancer. Her husband joined her in the United States in 2017; she cares for him because he has heart failure.
“Nearly every one of us from Africa, we know how to care for older adults,” she said.
Her daughter is now in the United States, while her son is still in Africa. Conteh said she sends money to him, her mother-in-law, and one of her sisters.
In the nursing home where Goodness and 89 other residents live, Conteh helps with daily tasks like dressing and eating, checks residents’ skin for signs of swelling or sores, and tries to help them avoid falling or getting disoriented. Of 102 employees in the building, broken up into eight residential wings called “small houses” and a wing for memory care, at least 72 were born abroad, Hutter said.
Donald Goodness grew up in Rochester, New York, and spent 25 years as rector of The Church of the Ascension in New York City, retiring in 1997. He and his late wife moved to Alexandria to be closer to their daughter, and in 2011 they moved into independent living at the Goodwin House. In 2023 he moved into one of the skilled nursing small houses, where Conteh started caring for him.
“I have a bad leg and I can’t stand on it very much, or I’d fall over,” he said. “She’s in there at 7:30 in the morning, and she helps me bathe.” Goodness said Conteh is exacting about cleanliness and will tell the housekeepers if his room is not kept properly.
Conteh said Goodness was withdrawn when he first arrived. “He don’t want to come out, he want to eat in his room,” she said. “He don’t want to be with the other people in the dining room, so I start making friends with him.”
She showed him a photo of Sierra Leone on her phone and told him of the weather there. He told her about his work at the church and how his wife did laundry for the choir. The breakthrough, she said, came one day when he agreed to lunch with her in the dining room. Long out of his shell, Goodness now sits on the community’s resident council and enjoys distributing the mail to other residents on his floor.
“The people that work in my building become so important to us,” Goodness said.
While Trump’s 2024 election campaign focused on foreigners here without authorization, his administration has broadened to target those legally here, including refugees who fled countries beset by wars or natural disasters. This month, the Department of Homeland Security revoked the work permits for migrants and refugees from Cuba, Haiti, Nicaragua, and Venezuela who arrived under a Biden-era program.
“I’ve just spent my morning firing good, honest people because the federal government told us that we had to,” Rachel Blumberg, president of the Toby & Leon Cooperman Sinai Residences of Boca Raton, a Florida retirement community, said in a video posted on LinkedIn. “I am so sick of people saying that we are deporting people because they are criminals. Let me tell you, they are not all criminals.”
At Goodwin House, Conteh is fearful for her fellow immigrants. Foreign workers at Goodwin rarely talk about their backgrounds. “They’re scared,” she said. “Nobody trusts anybody.” Her neighbors in her apartment complex fled the U.S. in December and returned to Sierra Leone after Trump won the election, leaving their children with relatives.
“If all these people leave the United States, they go back to Africa or to their various countries, what will become of our residents?” Conteh asked. “What will become of our old people that we’re taking care of?”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
This article first appeared on KFF Health News and is republished here under a Creative Commons license.
The post Dual Threats From Trump and GOP Imperil Nursing Homes and Their Foreign-Born Workers appeared first on kffhealthnews.org
Note: The following A.I. based commentary is not part of the original article, reproduced above, but is offered in the hopes that it will promote greater media literacy and critical thinking, by making any potential bias more visible to the reader –Staff Editor.
Political Bias Rating: Center-Left
This content primarily highlights concerns about the impact of restrictive immigration policies and Medicaid spending cuts proposed by the Trump administration and Republican lawmakers on the long-term care industry. It emphasizes the importance of immigrant workers in healthcare, the challenges that staffing shortages pose to patient care, and the potential negative effects of GOP policy proposals. The tone is critical of these policies while sympathetic toward immigrant workers and advocates for maintaining or increasing government support for healthcare funding. The framing aligns with a center-left perspective, focusing on social welfare, immigrant rights, and concern about the consequences of conservative economic and immigration policies without descending into partisan rhetoric.
Kaiser Health News
California’s Much-Touted IVF Law May Be Delayed Until 2026, Leaving Many in the Lurch
California lawmakers are poised to delay the state’s much-ballyhooed new law mandating in vitro fertilization insurance coverage for millions, set to take effect July 1. Gov. Gavin Newsom has asked lawmakers to push the implementation date to January 2026, leaving patients, insurers, and employers in limbo.
The law, SB 729, requires state-regulated health plans offered by large employers to cover infertility diagnosis and treatment, including IVF. Nine million people will qualify for coverage under the law. Advocates have praised the law as “a major win for Californians,” especially in making same-sex couples and aspiring single parents eligible, though cost concerns limited the mandate’s breadth.
People who had been planning fertility care based on the original timeline are now “left in a holding pattern facing more uncertainty, financial strain, and emotional distress,” Alise Powell, a director at Resolve: The National Infertility Association, said in a statement.
During IVF, a patient’s eggs are retrieved, combined with sperm in a lab, and then transferred to a person’s uterus. A single cycle can total around $25,000, out of reach for many. The California law requires insurers to cover up to three egg retrievals and an unlimited number of embryo transfers.
Not everyone’s coverage would be affected by the delay. Even if the law took effect July 1, it wouldn’t require IVF coverage to start until the month an employer’s contract renews with its insurer. Rachel Arrezola, a spokesperson for the California Department of Managed Health Care, said most of the employers subject to the law renew their contracts in January, so their employees would not be affected by a delay.
She declined to provide data on the percentage of eligible contracts that renew in July or later, which would mean those enrollees wouldn’t get IVF coverage until at least a full year from now, in July 2026 or later.
The proposed new implementation date comes amid heightened national attention on fertility coverage. California is now one of 15 states with an IVF mandate, and in February, President Donald Trump signed an executive order seeking policy recommendations to expand IVF access.
It’s the second time Newsom has asked lawmakers to delay the law. When the Democratic governor signed the bill in September, he asked the legislature to consider delaying implementation by six months. The reason, Newsom said then, was to allow time to reconcile differences between the bill and a broader effort by state regulators to include IVF and other fertility services as an essential health benefit, which would require the marketplace and other individual and small-group plans to provide the coverage.
Newsom spokesperson Elana Ross said the state needs more time to provide guidance to insurers on specific services not addressed in the law to ensure adequate and uniform coverage. Arrezola said embryo storage and donor eggs and sperm were examples of services requiring more guidance.
State Sen. Caroline Menjivar, a Democrat who authored the original IVF mandate, acknowledged a delay could frustrate people yearning to expand their families, but requested patience “a little longer so we can roll this out right.”
Sean Tipton, a lobbyist for the American Society for Reproductive Medicine, contended that the few remaining questions on the mandate did not warrant a long delay.
Lawmakers appear poised to advance the delay to a vote by both houses of the legislature, likely before the end of June. If a delay is approved and signed by the governor, the law would immediately be paused. If this does not happen before July 1, Arrezola said, the Department of Managed Health Care would enforce the mandate as it exists. All plans were required to submit compliance filings to the agency by March. Arrezola was unable to explain what would happen to IVF patients whose coverage had already begun if the delay passes after July 1.
The California Association of Health Plans, which opposed the mandate, declined to comment on where implementation efforts stand, although the group agrees that insurers need more guidance, spokesperson Mary Ellen Grant said.
Kaiser Permanente, the state’s largest insurer, has already sent employers information they can provide to their employees about the new benefit, company spokesperson Kathleen Chambers said. She added that eligible members whose plans renew on or after July 1 would have IVF coverage if implementation of the law is not delayed.
Employers and some fertility care providers appear to be grappling over the uncertainty of the law’s start date. Amy Donovan, a lawyer at insurance brokerage and consulting firm Keenan & Associates, said the firm has fielded many questions from employers about the possibility of delay. Reproductive Science Center and Shady Grove Fertility, major clinics serving different areas of California, posted on their websites that the IVF mandate had been delayed until January 2026, which is not yet the case. They did not respond to requests for comment.
Some infertility patients confused over whether and when they will be covered have run out of patience. Ana Rios and her wife, who live in the Central Valley, had been trying to have a baby for six years, dipping into savings for each failed treatment. Although she was “freaking thrilled” to learn about the new law last fall, Rios could not get clarity from her employer or health plan on whether she was eligible for the coverage and when it would go into effect, she said. The couple decided to go to Mexico to pursue cheaper treatment options.
“You think you finally have a helping hand,” Rios said of learning about the law and then, later, the requested delay. “You reach out, and they take it back.”
This article was produced by KFF Health News, which publishes California Healthline, an editorially independent service of the California Health Care Foundation.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
This article first appeared on KFF Health News and is republished here under a Creative Commons license.
The post California’s Much-Touted IVF Law May Be Delayed Until 2026, Leaving Many in the Lurch appeared first on kffhealthnews.org
Note: The following A.I. based commentary is not part of the original article, reproduced above, but is offered in the hopes that it will promote greater media literacy and critical thinking, by making any potential bias more visible to the reader –Staff Editor.
Political Bias Rating: Center-Left
This content is presented in a factual, balanced manner typical of center-left public policy reporting. It focuses on a progressive healthcare issue (mandated IVF insurance coverage) favorably highlighting benefits for diverse family structures and individuals, including same-sex couples and single parents, which often aligns with center-left values. At the same time, it includes perspectives from government officials, industry representatives, opponents, and patients, offering a nuanced view without overt ideological framing or partisan rhetoric. The emphasis on healthcare access, social equity, and patient impact situates the coverage within a center-left orientation.
-
News from the South - Arkansas News Feed6 days ago
Real-life Uncle Sam's descendants live in Arkansas
-
News from the South - Louisiana News Feed7 days ago
Her son faced 10 years behind bars; now she’s the one facing prison
-
News from the South - Arkansas News Feed7 days ago
Could roundabouts become more common than red lights?
-
News from the South - Georgia News Feed5 days ago
'Big Beautiful Bill' already felt at Georgia state parks | FOX 5 News
-
News from the South - Oklahoma News Feed6 days ago
LOFT report uncovers what led to multi-million dollar budget shortfall
-
News from the South - Alabama News Feed7 days ago
Alabama schools to lose $68 million in federal grants under Trump freeze
-
News from the South - Missouri News Feed7 days ago
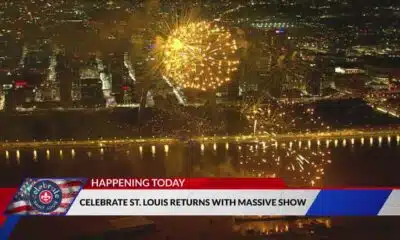
Celebrate St. Louis returns with new Superman-themed drone show
-
News from the South - Georgia News Feed6 days ago
Tropical Depression Three to bring rain, gusty winds to the CSRA this Fourth of July weekend