Mississippi Today
Faith, medical leaders to discuss expanding health care access at Gov. Tate Reeves’ home church


Galloway United Methodist, the downtown Jackson church where incumbent Republican Gov. Tate Reeves is a member, will host a series of lectures on how providing access to health care is a Christian value.
The featured speakers in late October are expected to tout Medicaid expansion, a federal-state program that would provide health care coverage to an estimated 300,000 poor, working Mississippians. Reeves, serving in two of the state’s top leadership roles for the past 12 years, has adamantly opposed the program, disparagingly likening it to “welfare expansion.”
That’s clearly not how the governor’s pastor sees it.
“Obviously, with a topic like ours, the issue of Medicaid expansion looms large,” Galloway Senior Pastor Cary Stockett said in an email to reporters announcing the lectures. “And I believe each of our speakers are in favor of Medicaid expansion. We do not look to it as a panacea, nor do we wish these conversations revolve around the legislative football that subject has become.
“So, while we will not avoid mention of Medicaid expansion, our purpose is to bring people of faith to see good healthcare as a corollary of Jesus’ command, to love your neighbor as yourself,” Stockett continued. “We want it understood that this is a kingdom of God issue, grossly ignored right in the middle of the Bible Belt. We want the people who quote John 3:16 to understand that it matters to Jesus that there are people (our Mississippi neighbors) without real access to good healthcare…and so it should matter to us, too.”
No doubt, Stockett had no intention of inserting himself into a political debate. In his announcement of the lectures, he certainly didn’t mention Reeves or the 2023 elections.
But as more Mississippians than ever are tuned in to the state’s worsening health care crisis — and as the lectures will be held right against the backdrop of the November governor’s election — the contrast in views is impossible to ignore.
The Galloway lectures will take place Oct. 27-28, just 10 days before the Nov. 7 general election. Reeves faces Democratic challenger Brandon Presley, who has made his strong support for Medicaid expansion a top issue of his campaign. Independent candidate Gwendolyn Gray, also on the ballot, supports expansion.
READ MORE: Brandon Presley again vows to expand Medicaid as Gov. Tate Reeves reiterates opposition
Reeves publicly touts his Christian values, regularly posting Bible verses to social media and discussing his faith on the campaign trail. He even hosted live-streamed prayer services on his Facebook page during the COVID-19 lockdowns. He was his “pleasure” to declare Christian Heritage Week of Sept. 21, which also happened to be the date of Yom Kippur, the day of atonement in the Jewish faith and the religion’s holiest day.
Though the governor speaks publicly of his religion and even his membership at Galloway, he has never publicly equated health care access with his faith.
Mississippi, which has the nation’s highest rate of people without health insurance, is one of just 10 states that has not expanded Medicaid, thus leaving more than $1 billion in federal money on the table annually. Reeves has gone out of his way for more than a decade to block it.
The state is also in the throes of a hospital financial crisis in which nearly half of rural hospitals are at risk of closure and even larger hospitals have been forced to slash services or lay off staff. The hospital crisis is exacerbated by the fact that hospitals themselves must cover the health care service costs for uninsured patients.
After years of inaction on the health care crisis, Reeves last week announced a plan that would provide additional funding to hospitals. Much of the new funding would come from an increase in hospital taxes that would then allow the state to draw down additional federal funding through a Medicaid reimbursement program.
Experts say the Reeves proposal will help hospitals, but they said the plan will provide no relief to uninsured Mississippians. In the press conference announcing his plan, Reeves was asked why he supported drawing down federal money to help hospitals under his plan but opposed drawing down federal money to help uninsured patients via Medicaid expansion.
“We need more people in the workforce,” Reeves said. “… So adding 300,000 able-bodied Mississippians to the welfare rolls, I would argue, is a bad idea.”
READ MORE: Gov. Reeves announces 11th hour plan for hospital crisis. Opponents pan it as ‘too little, too Tate’
A study by the Kaiser Family Foundation found that 61% of Medicaid recipients work and another 30% of recipients are students, people who are disabled, or caregivers. Medicaid expansion is designed, in part, to provide health insurance to people who work in jobs where their employers do not provide health insurance and they do not earn enough to afford private insurance.
“Until Medicaid is expanded, Mississippians will continue to pay the price in lost dollars, lost jobs, and lost lives,” Roy Mitchell, executive director of the Mississippi Health Advocacy Program, said of Reeves’ recent announcement. “This is a state executive branch, making a health policy decision based largely in myth and an ideological belief structure. The reality is hundreds of thousands of Mississippians are not paid enough to afford health insurance coverage.”
Without question, the moral arguments being made by Stockett, Mitchell and others for health care access for poor Mississippians will continue regardless of the outcome of the 2023 governor’s election.
The Galloway lecture series will begin Oct. 27 at 5:30 p.m. and Oct. 28 at 8:30 a.m. at Galloway, located a block from the Governor’s Mansion in downtown Jackson. The lecturers are:
- Rev. Chuck Poole, former pastor of Northminster Baptist Church in Jackson and now working with Together for Hope.
- Dr. Dan Jones, former chancellor of the University of Mississippi and former dean of medicine at the University of Mississippi Medical Center.
- Rev. Jason Coker, president and director of Together for Hope, a collation working to improve the standard of living in rural areas such as the Delta and Appalachia.
- Dr. Sandra Melvin, a public health doctor and chief executive officer of the Institute for the Advancement of Minority Health.
- Von Gordon, executive director of the Alluvial Collection, previously known as the William Winter Institute.
- Dr. Michelle Owens, an OB-GYN in Jackson and the president of the Mississippi State Board of Medical Licensure.
The event is part of Galloway’s T.W. Lewis Lecture Series on Jesus and a Just Society. The series was started by an anonymous donor in honor of T.W. Lewis, an ordained elder in the Mississippi Conference of the United Methodist Church and professor emeritus of religious studies at Millsaps College — the governor’s alma mater.
READ MORE: Experts say Gov. Tate Reeves’ plan will help hospitals, but not uninsured Mississippians
This article first appeared on Mississippi Today and is republished here under a Creative Commons license.
Did you miss our previous article…
https://www.biloxinewsevents.com/?p=292112
Mississippi Today
Speaker White wants Christmas tree projects bill included in special legislative session

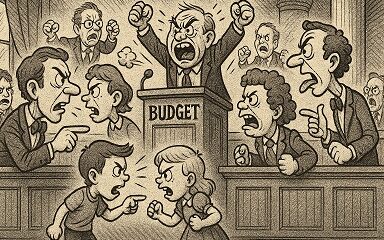
House Speaker Jason White sent a terse letter to Lt. Gov. Delbert Hosemann on Thursday, saying House leaders are frustrated with Senate leaders refusing to discuss a “Christmas tree” bill spending millions on special projects across the state.
The letter signals the two Republican leaders remain far apart on setting an overall $7 billion state budget. Bickering between the GOP leaders led to a stalemate and lawmakers ending their regular 2025 session without setting a budget. Gov. Tate Reeves plans to call them back into special session before the new budget year starts July 1 to avoid a shutdown, but wants them to have a budget mostly worked out before he does so.
White’s letter to Hosemann, which contains words in all capital letters that are underlined and italicized, said that the House wants to spend cash reserves on projects for state agencies, local communities, universities, colleges, and the Mississippi Department of Transportation.
“We believe the Senate position to NOT fund any local infrastructure projects is unreasonable,” White wrote.
The speaker in his letter noted that he and Hosemann had a meeting with the governor on Tuesday. Reeves, according to the letter, advised the two legislative leaders that if they couldn’t reach an agreement on how to disburse the surplus money, referred to as capital expense money, they should not spend any of it on infrastructure.
A spokesperson for Hosemann said the lieutenant governor has not yet reviewed the letter, and he was out of the office on Thursday working with a state agency.
“He is attending Good Friday services today, and will address any correspondence after the celebration of Easter,” the spokesperson said.
Hosemann has recently said the Legislature should set an austere budget in light of federal spending cuts coming from the Trump administration, and because state lawmakers this year passed a measure to eliminate the state income tax, the source of nearly a third of the state’s operating revenue.
Lawmakers spend capital expense money for multiple purposes, but the bulk of it — typically $200 million to $400 million a year — goes toward local projects, known as the Christmas Tree bill. Lawmakers jockey for a share of the spending for their home districts, in a process that has been called a political spoils system — areas with the most powerful lawmakers often get the largest share, not areas with the most needs. Legislative leaders often use the projects bill as either a carrot or stick to garner votes from rank and file legislators on other issues.
A Mississippi Today investigation last year revealed House Ways and Means Chairman Trey Lamar, a Republican from Sentobia, has steered tens of millions of dollars in Christmas tree spending to his district, including money to rebuild a road that runs by his north Mississippi home, renovate a nearby private country club golf course and to rebuild a tiny cul-de-sac that runs by a home he has in Jackson.
There is little oversight on how these funds are spent, and there is no requirement that lawmakers disburse the money in an equal manner or based on communities’ needs.
In the past, lawmakers borrowed money for Christmas tree bills. But state coffers have been full in recent years largely from federal pandemic aid spending, so the state has been spending its excess cash. White in his letter said the state has “ample funds” for a special projects bill.
“We, in the House, would like to sit down and have an agreement with our Senate counterparts on state agency Capital Expenditure spending AND local projects spending,” White wrote. “It is extremely important to our agencies and local governments. The ball is in your court, and the House awaits your response.”
This article first appeared on Mississippi Today and is republished here under a Creative Commons Attribution-NoDerivatives 4.0 International License.
Mississippi Today
Advocate: Election is the chance for Jackson to finally launch in the spirit of Blue Origin

Editor’s note: This essay is part of Mississippi Today Ideas, a platform for thoughtful Mississippians to share fact-based ideas about our state’s past, present and future. You can read more about the section here.
As the world recently watched the successful return of Blue Origin’s historic all-women crew from space, Jackson stands grounded. The city is still grappling with problems that no rocket can solve.
But the spirit of that mission — unity, courage and collective effort — can be applied right here in our capital city. Instead of launching away, it is time to launch together toward a more just, functioning and thriving Jackson.
The upcoming mayoral runoff election on April 22 provides such an opportunity, not just for a new administration, but for a new mindset. This isn’t about endorsements. It’s about engagement.
It’s a moment for the people of Jackson and Hinds County to take a long, honest look at ourselves and ask if we have shown up for our city and worked with elected officials, instead of remaining at odds with them.
It is time to vote again — this time with deeper understanding and shared responsibility. Jackson is in crisis — and crisis won’t wait.
According to the U.S. Census projections, Jackson is the fastest-shrinking city in the United States, losing nearly 4,000 residents in a single year. That kind of loss isn’t just about numbers. It’s about hope, resources, and people’s decision to give up rather than dig in.
Add to that the long-standing issues: a crippled water system, public safety concerns, economic decline and a sense of division that often pits neighbor against neighbor, party against party and race against race.
Mayor Chokwe Antar Lumumba has led through these storms, facing criticism for his handling of the water crisis, staffing issues and infrastructure delays. But did officials from the city, the county and the state truly collaborate with him or did they stand at a distance, waiting to assign blame?
On the flip side, his runoff opponent, state Sen. John Horhn, who has served for more than three decades, is now seeking to lead the very city he has represented from the Capitol. Voters should examine his legislative record and ask whether he used his influence to help stabilize the administration or only to position himself for this moment.
Blaming politicians is easy. Building cities is hard. And yet that is exactly what’s needed. Jackson’s future will not be secured by a mayor alone. It will take so many of Jackson’s residents — voters, business owners, faith leaders, students, retirees, parents and young people — to move this city forward. That’s the liftoff we need.
It is time to imagine Jackson as a capital city where clean, safe drinking water flows to every home — not just after lawsuits or emergencies, but through proactive maintenance and funding from city, state and federal partnerships. The involvement of the U.S. Environmental Protection Agency in the effort to improve the water system gives the city leverage.
Public safety must be a guarantee and includes prevention, not just response, with funding for community-based violence interruption programs, trauma services, youth job programs and reentry support. Other cities have done this and it’s working.
Education and workforce development are real priorities, preparing young people not just for diplomas but for meaningful careers. That means investing in public schools and in partnerships with HBCUs, trade programs and businesses rooted right here.
Additionally, city services — from trash collection to pothole repair — must be reliable, transparent and equitable, regardless of zip code or income. Seamless governance is possible when everyone is at the table.
Yes, democracy works because people show up. Not just to vote once, but to attend city council meetings, serve on boards, hold leaders accountable and help shape decisions about where resources go.
This election isn’t just about who gets the title of mayor. It’s about whether Jackson gets another chance at becoming the capital city Mississippi deserves — a place that leads by example and doesn’t lag behind.
The successful Blue Origin mission didn’t happen by chance. It took coordinated effort, diverse expertise and belief in what was possible. The same is true for this city.
We are not launching into space. But we can launch a new era marked by cooperation over conflict, and by sustained civic action over short-term outrage.
On April 22, go vote. Vote not just for a person, but for a path forward because Jackson deserves liftoff. It starts with us.
Pauline Rogers is a longtime advocate for criminal justice reform and the founder of the RECH Foundation, an organization dedicated to supporting formerly incarcerated individuals as they reintegrate into society. She is a Transformative Justice Fellow through The OpEd Project Public Voices Fellowship.
This article first appeared on Mississippi Today and is republished here under a Creative Commons Attribution-NoDerivatives 4.0 International License.![]()
Mississippi Today
On this day in 1959, students marched for integrated schools

April 18, 1959

About 26,000 students took part in the Youth March for Integrated Schools in Washington, D.C. They heard speeches by Martin Luther King Jr., A. Phillip Randolph and NAACP leader Roy Wilkins.
In advance of the march, false accusations were made that Communists had infiltrated the group. In response, the civil rights leaders put out a statement: “The sponsors of the March have not invited Communists or communist organizations. Nor have they invited members of the Ku Klux Klan or the White Citizens’ Council. We do not want the participation of these groups, nor of individuals or other organizations holding similar views.”
After the march, a delegation of students went to present their demands to President Eisenhower, only to be told by his deputy assistant that “the president is just as anxious as they are to see an America where discrimination does not exist, where equality of opportunity is available to all.”
King praised the students, saying, “In your great movement to organize a march for integrated schools, you have awakened on hundreds of campuses throughout the land a new spirit of social inquiry to the benefit of all Americans.”
This article first appeared on Mississippi Today and is republished here under a Creative Commons Attribution-NoDerivatives 4.0 International License.![]()
-

 Mississippi Today6 days ago
Mississippi Today6 days agoOn this day in 1873, La. courthouse scene of racial carnage
-

 Local News7 days ago
Local News7 days agoAG Fitch and Children’s Advocacy Centers of Mississippi Announce Statewide Protocol for Child Abuse Response
-

 Mississippi Today6 days ago
Mississippi Today6 days agoLawmakers used to fail passing a budget over policy disagreement. This year, they failed over childish bickering.
-

 Local News6 days ago
Local News6 days agoSouthern Miss Professor Inducted into U.S. Hydrographer Hall of Fame
-

 News from the South - Alabama News Feed4 days ago
News from the South - Alabama News Feed4 days agoFoley man wins Race to the Finish as Kyle Larson gets first win of 2025 Xfinity Series at Bristol
-

 News from the South - North Carolina News Feed7 days ago
News from the South - North Carolina News Feed7 days agoHelene: Renewed focus on health of North Carolina streams | North Carolina
-

 News from the South - Alabama News Feed4 days ago
News from the South - Alabama News Feed4 days agoFederal appeals court upholds ruling against Alabama panhandling laws
-

 Our Mississippi Home7 days ago
Our Mississippi Home7 days agoFood Chain Drama | Our Mississippi Home