Mississippi Today
New Health Department program puts nurses in the homes of high-risk moms, babies in Mississippi

Through a partnership between the state Health Department and the state Division of Medicaid, Healthy Moms, Healthy Babies program places registered nurse case managers in the homes of pregnant mothers undergoing high-risk pregnancies.
Since launching, it has expanded to 23 full-time nurses and 17 part-time nurses providing services to about 640 patients around the state.
State Health Officer Dr. Daniel Edney said the program is “plugging the gap” by bringing resources to small rural communities that aren’t there.
“With limited resources for mothers and babies, a lot of our efforts are going to be directed to our highest impacted areas to help the folks in the most desperate need the fastest,” Edney said.
The way resources are distributed across the state – sparsely in rural and remote areas but plentiful in certain others – means the program must take a targeted approach.
“We can not look at Mississippi as one organism. We are really six different regions when it comes to public health in terms of populations, demographics, resources available and challenges,” Edney explained. “I have to have different strategies for different areas. The one-size fits all strategy won’t work.”
Dr. Justin Turner, chief medical officer at the state Health Department, witnessed personally how important access to quality health care for mothers is.
Turner’s wife made 23 total visits to five different hospitals or emergency rooms during her last two pregnancies.
Seven out of 23 of those visits came during her pregnancy five years ago, and the remainder of the visits came during their second pregnancy in August 2022. During her last pregnancy, she experienced “uncharacteristic pain” around month five, requiring her to be supervised by her family 24 hours a day until she gave birth.
The pain would spiral out of control resulting in psychogenic nonepileptic seizures (PNES), previously known as pseudoseizures – emotional and stress-related episodes similar to epileptic seizures but not of neurological origin.
As the number of trips increased, Turner said he had a tough time reassuring his family and himself.
“I was thinking, 'how do I continue to do what I’m supposed to do as the chief medical officer and help assist the state as a whole, when I can’t even help my wife at home?'” Turner told Mississippi Today.
For Black women in Mississippi, the pregnancy-related mortality rate increased from 51.9 to 65.1 deaths per 100,000 live births, quadruple the rate of white women (16.2). With this data in mind, fears of the worst outcome flooded both Turner and his wife’s minds.
“It was natural for me to think that my wife was going to be another statistic,” Turner explained. “She would ask me things like, ‘Baby, am I going to die?’”
The pregnancy remained a challenge until the day that she delivered their child by cesarean section. Every day prior to her being pregnant was “a day of misery,” Turner said. After delivery, his wife never experienced another pseudoseizure episode.
Turner said fortunately for his wife, she had a husband who is a doctor, an OB-GYN, support from family and friends, and a great health care team.
However, he couldn't help but think of how many mothers in Mississippi lack support. Turner said the Healthy Moms, Healthy Babies program aims to add emotional support for mothers who may be in need of it.
“For a lot of women, they benefit from the nurturing and feeling like someone is listening,” Turner continued. “The more people that’s on their team, the better it helps them to endure the process of pregnancy itself.”
As services are being provided to participants, Turner said the health department, stakeholders, policy makers and community members must collaborate to improve outcomes for mothers and their babies.
“We need to find common ground in the areas that we can improve and make sure that we are providing our moms and babies a decent chance at having a healthy pregnancy and coming into this world,” Turner said.
As a Medicaid-reimbursed program, Healthy Moms, Healthy Babies allows mothers to receive monthly targeted case management, health education, and assessments by nurses, social workers and nutritionists at no direct cost to them.
For moms with Medicaid, the services are reimbursed. Edney said the program works with uninsured moms to help them enroll in Medicaid or, if they are not eligible, will provide the services for free.
The Mississippi State Health Department declined Mississippi Today's request to interview a mother who has participated in the program.
After making contact with a mom in need, the nurse consults with the mother’s doctor, who shares why she may be considered high-risk. Common high-risk conditions include preterm labor, diabetes, multiple pregnancy losses and starting prenatal care late.
The nurse then works to mitigate her symptoms by going to the mother's home and pairing her with a multidisciplinary team of resources, such as social workers and nutritionists.
The team of health care workers educate her on the importance of prenatal care, diet plans and how to limit her chances of becoming high-risk in the future. Edney said the program is “working aggressively” to support affected Medicaid moms.
“In our last reporting from the maternal mortality review committee, 87% of deaths were Medicaid moms, and out of all of our maternal deaths, 80% were preventable,” Edney told Mississippi Today. “That is unacceptable.”
Currently, 86% of the participating mothers are Medicaid beneficiaries.
Healthy Moms, Healthy Babies monitors not only high-risk mothers but also high-risk babies up to one year of age.

A baby is considered high risk if they are born prior to 37 weeks of gestation, weigh less than 5 pounds 8 ounces at birth, have genetic disorders, experience nutritional deficiencies, infections, or live in unsafe conditions among other factors as well.
The average age of infants enrolled in the program is less than one month old.
The goal of the program is to increase the infant's chances of survival, Edney said. Mississippi leads the nation in its rate of infant mortality.
“I know that if we continue doing what we are doing, nothing is going to change. So, if we all agree we have a problem, which I think everybody does, then this has got to change,” Edney stated. “I don’t have to convince anybody that being 50th in the nation for dead babies is a good thing, because it isn’t.”
The Health Department plans to expand the program so that more women and babies in rural communities have access to necessary care.
Around 35% of babies were born to women living in rural counties of the state, but only a quarter of maternity care providers practice there, according to the latest March of Dimes’ report.
Jillian Harper-Peavy, the state program director for Healthy Moms, Healthy Babies, said partnerships with different individuals and organizations are critical for the program to expand.

Those organizations include community health centers; hospitals; OB-GYN offices; pediatricians; managed care organizations; and other maternal and child health programs.
“We are prioritizing outreach and engagement of patients continually, as we do want to see the program serve more pregnant women and infants,” Harper-Peavy continued. “As additional patients are enrolled, we will continue to assess our staffing capacity and plan accordingly.”
However, financial constraints have hindered its expansion.
Earlier this year, Edney asked lawmakers to fund $9 million to hire nurses needed to fully staff county health departments and Healthy Moms, Healthy Babies. The request was denied.
Now, Edney said he is seeking to redirect the funding he has and cut back in every department possible to hire the 100 or so nurses he’s identified as potential job candidates.
“I’m trying to provide core public health services around this state with a battered workforce,” Edney explained. “I try to get people to understand that while everybody else may be over COVID-19, the health department is not. We were beaten to pieces, and we’re working hard to rebuild our workforce with the resources that we have.”
Susan Bates, nurse team lead in the northeastern region of the state, manages a team of nurses who serve patients in 11 counties, seven of which are maternal health deserts: Marshall, Benton, Tippah, Pontotoc, Prentiss, Tishomingo and Itawamba.
These counties have no hospitals or birthing centers that provide obstetric care, and no practicing OB-GYNs or certified nurse midwives.
Across the state, 51.2% of counties are defined as maternity care deserts, compared to 32.6% nationally.
Bates, who cares for an average of six to 10 mothers and babies each day, has encountered women experiencing preterm labor, preterm delivery, preeclampsia, anxiety and depression. She’s also cared for premature and low-birthweight babies.
With more than 26 years of nursing experience, Bates said she aims to make every patient feel respected, valued and heard. Her approach is to listen, understand and “not just focus on checking a box.”
“I feel that it is important to establish a relationship of trust between the mother and her doctors that way we can promote and foster communication. This allows us to provide a more comprehensive care and therefore improve our patients’ outcomes,” Bates continued. “So, when we meet our patients' needs, consistently and correctly, they develop trust in us as their caregiver.”
The Corinth native previously worked for the Mississippi State Health Department for 11 years as a public health nurse, promoting and protecting the health of populations using knowledge from nursing, social and public health science.
Bates, who is certified in pediatric advanced life support and neonatal advanced life support, said caring for high-risk mothers and babies requires a calm demeanor to help the family through what can be a scary time.
“If you look at the big picture, then it may seem overwhelming, but we can’t be stopped by that. We have to know that what we are doing makes a difference to each patient,” Bates explained. “One life at a time, we’re making a difference.”
Edney said that scoring poorly in maternal and infant mortality is a “heavy burden” that requires a “heavy lift” to flip the negative trend to a positive one.
“It’ll take years, but with the work that we’re going to do with the agency, I’m convinced that we will not only get off the bottom with infant mortality,” Edney stated, “we will get off the radar.”
This article first appeared on Mississippi Today and is republished here under a Creative Commons license.
Mississippi Today
Mississippi prepares for another execution
The Mississippi Supreme Court has set the execution of a man who kidnapped and murdered a 20-year-old community college student in north Mississippi 30 years ago.
Charles Ray Crawford, 59, is set to be executed Oct. 15 at the Mississippi State Penitentiary at Parchman, after multiple requests by the attorney general’s office.
Eight justices joined the majority opinion to set the execution, concluding that Crawford has exhausted all state and federal legal remedies. Mississippi Supreme Court Justice T. Kenneth Griffis Jr. wrote the Friday opinion. Justice David Sullivan did not participate.
However, Kristy Noble with the Mississippi Office of Capital Post-Conviction Counsel released a statement saying it will file another appeal with the U.S. Supreme Court.
“”Mr. Crawford’s inexperienced trial counsel conceded his guilt to the jury — against Mr.
Crawford’s timely and repeated objections,” Noble said in the statement. “Mr. Crawford told his counsel to pursue a not guilty verdict. Counsel did just the opposite, which is precisely what the U.S. Supreme Court says counsel cannot do,” Noble said in the statement.
“A trial like Mr. Crawford’s – one where counsel concedes guilt over his client’s express wishes – is essentially no trial at all.”
Last fall, Crawford’s attorneys asked the court not to set an execution date because he hadn’t exhausted appeal efforts in federal court to challenge a rape conviction that is not tied to his death sentence. In June, the U.S. Supreme Court declined to take up Crawford’s case.
A similar delay occurred a decade ago, when the AG’s office asked the court to reset Crawford’s execution date, but that was denied because efforts to appeal his unrelated rape conviction were still pending.
After each unsuccessful filing, the attorney general’s office asked the Mississippi Supreme Court to set Crawford’s execution date.
On Friday, the court also denied Crawford’s third petition for post-conviction relief and a request for oral argument. It accepted the state’s motion to dismiss the petition. Seven justices concurred and Justice Leslie King concurred in result only. Again, Justice Sullivan did not participate.
Crawford was convicted and sentenced to death in Lafayette County for the 1993 rape and murder of North Mississippi Community College student Kristy Ray.
Days before he was set to go to trial on separate aggravated assault and rape charges, he kidnapped Ray from her parents’ Tippah County home, leaving ransom notes. Crawford took Ray to an abandoned barn where he stabbed her, and his DNA was found on her, indicating he sexually assaulted her, according to court records.
Crawford told police he had blackouts and only remembered parts of the crime, but not killing Ray. Later he admitted “he must of killed her” and led police to Ray’s body, according to court records.
At his 1994 trial he presented an insanity defense, including that he suffered from psychogenic amnesia – periods of time lapse without memory. Medical experts who provided rebuttal testimony said Crawford didn’t have psychogenic amnesia and didn’t show evidence of bipolar illness.
The last person executed in Mississippi was Richard Jordan in June, previously the state’s oldest and longest serving person on death row.
There are 36 people on death row, according to records from the Mississippi Department of Corrections.
Update 9/15/25: This story has been updated to include a response from the Mississippi Office of Capital Post-Conviction Counsel
This article first appeared on Mississippi Today and is republished here under a Creative Commons Attribution-NoDerivatives 4.0 International License.
The post Mississippi prepares for another execution appeared first on mississippitoday.org
Note: The following A.I. based commentary is not part of the original article, reproduced above, but is offered in the hopes that it will promote greater media literacy and critical thinking, by making any potential bias more visible to the reader –Staff Editor.
Political Bias Rating: Centrist
The article presents a factual and balanced account of the legal proceedings surrounding a scheduled execution in Mississippi. It includes perspectives from both the state’s attorney general’s office and the defense counsel, without using emotionally charged language or advocating for a particular political stance. The focus on legal details and court decisions reflects a neutral, informative approach typical of centrist reporting.
Mississippi Today
Presidents are taking longer to declare major natural disasters. For some, the wait is agonizing
TYLERTOWN — As an ominous storm approached Buddy Anthony’s one-story brick home, he took shelter in his new Ford F-250 pickup parked under a nearby carport.
Seconds later, a tornado tore apart Anthony’s home and damaged the truck while lifting it partly in the air. Anthony emerged unhurt. But he had to replace his vehicle with a used truck that became his home while waiting for President Donald Trump to issue a major disaster declaration so that federal money would be freed for individuals reeling from loss. That took weeks.
“You wake up in the truck and look out the windshield and see nothing. That’s hard. That’s hard to swallow,” Anthony said.
Disaster survivors are having to wait longer to get aid from the federal government, according to a new Associated Press analysis of decades of data. On average, it took less than two weeks for a governor’s request for a presidential disaster declaration to be granted in the 1990s and early 2000s. That rose to about three weeks during the past decade under presidents from both major parties. It’s taking more than a month, on average, during Trump’s current term, the AP found.
The delays mean individuals must wait to receive federal aid for daily living expenses, temporary lodging and home repairs. Delays in disaster declarations also can hamper recovery efforts by local officials uncertain whether they will receive federal reimbursement for cleaning up debris and rebuilding infrastructure. The AP collaborated with Mississippi Today and Mississippi Free Press on the effects of these delays for this report.
“The message that I get in the delay, particularly for the individual assistance, is that the federal government has turned its back on its own people,” said Bob Griffin, dean of the College of Emergency Preparedness, Homeland Security and Cybersecurity at the University at Albany in New York. “It’s a fundamental shift in the position of this country.”
The wait for disaster aid has grown as Trump remakes government
The Federal Emergency Management Agency often consults immediately with communities to coordinate their initial disaster response. But direct payments to individuals, nonprofits and local governments must wait for a major disaster declaration from the president, who first must receive a request from a state, territory or tribe. Major disaster declarations are intended only for the most damaging events that are beyond the resources of states and local governments.
Trump has approved more than two dozen major disaster declarations since taking office in January, with an average wait of almost 34 days after a request. That ranged from a one-day turnaround after July’s deadly flash flooding in Texas to a 67-day wait after a request for aid because of a Michigan ice storm. The average wait is up from a 24-day delay during his first term and is nearly four times as long as the average for former Republican President George H.W. Bush, whose term from 1989-1993 coincided with the implementation of a new federal law setting parameters for disaster determinations.
The delays have grown over time, regardless of the party in power. Former Democratic President Joe Biden, in his last year in office, averaged 26 days to declare major disasters — longer than any year under former Democratic President Barack Obama.

FEMA did not respond to the AP’s questions about what factors are contributing to the trend.
Others familiar with FEMA noted that its process for assessing and documenting natural disasters has become more complex over time. Disasters have also become more frequent and intense because of climate change, which is mostly caused by the burning of fuels such as gas, coal and oil.
The wait for disaster declarations has spiked as Trump’s administration undertakes an ambitious makeover of the federal government that has shed thousands of workers and reexamined the role of FEMA. A recently published letter from current and former FEMA employees warned the cuts could become debilitating if faced with a large-enough disaster. The letter also lamented that the Trump administration has stopped maintaining or removed long-term planning tools focused on extreme weather and disasters.
Shortly after taking office, Trump floated the idea of “getting rid” of FEMA, asserting: “It’s very bureaucratic, and it’s very slow.”
FEMA’s acting chief suggested more recently that states should shoulder more responsibility for disaster recovery, though FEMA thus far has continued to cover three-fourths of the costs of public assistance to local governments, as required under federal law. FEMA pays the full cost of its individual assistance.
Former FEMA Administrator Pete Gaynor, who served during Trump’s first term, said the delay in issuing major disaster declarations likely is related to a renewed focus on making sure the federal government isn’t paying for things state and local governments could handle.
“I think they’re probably giving those requests more scrutiny,” Gaynor said. “And I think it’s probably the right thing to do, because I think the (disaster) declaration process has become the ‘easy button’ for states.”
The Associated Press on Monday received a statement from White House spokeswoman Abigail Jackson in response to a question about why it is taking longer to issue major natural disaster declarations:
“President Trump provides a more thorough review of disaster declaration requests than any Administration has before him. Gone are the days of rubber stamping FEMA recommendations – that’s not a bug, that’s a feature. Under prior Administrations, FEMA’s outsized role created a bloated bureaucracy that disincentivized state investment in their own resilience. President Trump is committed to right-sizing the Federal government while empowering state and local governments by enabling them to better understand, plan for, and ultimately address the needs of their citizens. The Trump Administration has expeditiously provided assistance to disasters while ensuring taxpayer dollars are spent wisely to supplement state actions, not replace them.”

In Mississippi, frustration festered during wait for aid
The tornado that struck Anthony’s home in rural Tylertown on March 15 packed winds up to 140 mph. It was part of a powerful system that wrecked homes, businesses and lives across multiple states.
Mississippi’s governor requested a federal disaster declaration on April 1. Trump granted that request 50 days later, on May 21, while approving aid for both individuals and public entities.
On that same day, Trump also approved eight other major disaster declarations for storms, floods or fires in seven other states. In most cases, more than a month had passed since the request and about two months since the date of those disasters.
If a presidential declaration and federal money had come sooner, Anthony said he wouldn’t have needed to spend weeks sleeping in a truck before he could afford to rent the trailer where he is now living. His house was uninsured, Anthony said, and FEMA eventually gave him $30,000.
In nearby Jayess in Lawrence County, Dana Grimes had insurance but not enough to cover the full value of her damaged home. After the eventual federal declaration, Grimes said FEMA provided about $750 for emergency expenses, but she is now waiting for the agency to determine whether she can receive more.

“We couldn’t figure out why the president took so long to help people in this country,” Grimes said. “I just want to tie up strings and move on. But FEMA — I’m still fooling with FEMA.”
Jonathan Young said he gave up on applying for FEMA aid after the Tylertown tornado killed his 7-year-old son and destroyed their home. The process seemed too difficult, and federal officials wanted paperwork he didn’t have, Young said. He made ends meet by working for those cleaning up from the storm.
“It’s a therapy for me,” Young said, “to pick up the debris that took my son away from me.”
Historically, presidential disaster declarations containing individual assistance have been approved more quickly than those providing assistance only to public entities, according to the AP’s analysis. That remains the case under Trump, though declarations for both types are taking longer.
About half the major disaster declarations approved by Trump this year have included individual assistance.
Some people whose homes are damaged turn to shelters hosted by churches or local nonprofit organizations in the initial chaotic days after a disaster. Others stay with friends or family or go to a hotel, if they can afford it.
But some insist on staying in damaged homes, even if they are unsafe, said Chris Smith, who administered FEMA’s individual assistance division under three presidents from 2015-2022. If homes aren’t repaired properly, mold can grow, compounding the recovery challenges.

That’s why it’s critical for FEMA’s individual assistance to get approved quickly — ideally, within two weeks of a disaster, said Smith, who’s now a disaster consultant for governments and companies.
“You want to keep the people where they are living. You want to ensure those communities are going to continue to be viable and recover,” Smith said. “And the earlier that individual assistance can be delivered … the earlier recovery can start.”
In the periods waiting for declarations, the pressure falls on local officials and volunteers to care for victims and distribute supplies.
In Walthall County, where Tylertown is, insurance agent Les Lampton remembered watching the weather news as the first tornado missed his house by just an eighth of a mile. Lampton, who moonlights as a volunteer firefighter, navigated the collapsed trees in his yard and jumped into action. About 45 minutes later, the second tornado hit just a mile away.
“It was just chaos from there on out,” Lampton said.
Walthall County, with a population of about 14,000, hasn’t had a working tornado siren in about 30 years, Lampton said. He added there isn’t a public safe room in the area, although a lot of residents have ones in their home.
Rural areas with limited resources are hit hard by delays in receiving funds through FEMA’s public assistance program, which, unlike individual assistance, only reimburses local entities after their bills are paid. Long waits can stoke uncertainty and lead cost-conscious local officials to pause or scale-back their recovery efforts.

In Walthall County, officials initially spent about $700,000 cleaning up debris, then suspended the cleanup for more than a month because they couldn’t afford to spend more without assurance they would receive federal reimbursement, said county emergency manager Royce McKee. Meanwhile, rubble from splintered trees and shattered homes remained piled along the roadside, creating unsafe obstacles for motorists and habitat for snakes and rodents.
When it received the federal declaration, Walthall County took out a multimillion-dollar loan to pay contractors to resume the cleanup.
“We’re going to pay interest and pay that money back until FEMA pays us,” said Byran Martin, an elected county supervisor. “We’re hopeful that we’ll get some money by the first of the year, but people are telling us that it could be [longer].”
Lampton, who took after his father when he joined the volunteer firefighters 40 years ago, lauded the support of outside groups such as Cajun Navy, Eight Days of Hope, Samaritan’s Purse and others. That’s not to mention the neighbors who brought their own skid steers and power saws to help clear trees and other debris, he added.
“That’s the only thing that got us through this storm, neighbors helping neighbors,” Lampton said. “If we waited on the government, we were going to be in bad shape.”
Lieb reported from Jefferson City, Missouri, and Wildeman from Hartford, Connecticut.
Update 98/25: This story has been updated to include a White House statement released after publication.
This article first appeared on Mississippi Today and is republished here under a Creative Commons Attribution-NoDerivatives 4.0 International License.
The post Presidents are taking longer to declare major natural disasters. For some, the wait is agonizing appeared first on mississippitoday.org
Note: The following A.I. based commentary is not part of the original article, reproduced above, but is offered in the hopes that it will promote greater media literacy and critical thinking, by making any potential bias more visible to the reader –Staff Editor.
Political Bias Rating: Center-Left
This article presents a critical view of the Trump administration’s handling of disaster declarations, highlighting delays and their negative impacts on affected individuals and communities. It emphasizes concerns about government downsizing and reduced federal support, themes often associated with center-left perspectives that favor robust government intervention and social safety nets. However, it also includes statements from Trump administration officials defending their approach, providing some balance. Overall, the tone and framing lean slightly left of center without being overtly partisan.
Mississippi Today
Northeast Mississippi speaker and worm farmer played key role in Coast recovery after Hurricane Katrina
The 20th anniversary of Hurricane Katrina slamming the Mississippi Gulf Coast has come and gone, rightfully garnering considerable media attention.
But still undercovered in the 20th anniversary saga of the storm that made landfall on Aug. 29, 2005, and caused unprecedented destruction is the role that a worm farmer from northeast Mississippi played in helping to revitalize the Coast.
House Speaker Billy McCoy, who died in 2019, was a worm farmer from the Prentiss, not Alcorn County, side of Rienzi — about as far away from the Gulf Coast as one could be in Mississippi.
McCoy grew other crops, but a staple of his operations was worm farming.
Early after the storm, the House speaker made a point of touring the Coast and visiting as many of the House members who lived on the Coast as he could to check on them.
But it was his action in the forum he loved the most — the Mississippi House — that is credited with being key to the Coast’s recovery.
Gov. Haley Barbour had called a special session about a month after the storm to take up multiple issues related to Katrina and the Gulf Coast’s survival and revitalization. The issue that received the most attention was Barbour’s proposal to remove the requirement that the casinos on the Coast be floating in the Mississippi Sound.
Katrina wreaked havoc on the floating casinos, and many operators said they would not rebuild if their casinos had to be in the Gulf waters. That was a crucial issue since the casinos were a major economic engine on the Coast, employing an estimated 30,000 in direct and indirect jobs.
It is difficult to fathom now the controversy surrounding Barbour’s proposal to allow the casinos to locate on land next to the water. Mississippi’s casino industry that was birthed with the early 1990s legislation was still new and controversial.
Various religious groups and others had continued to fight and oppose the casino industry and had made opposition to the expansion of gambling a priority.
Opposition to casinos and expansion of casinos was believed to be especially strong in rural areas, like those found in McCoy’s beloved northeast Mississippi. It was many of those rural areas that were the homes to rural white Democrats — now all but extinct in the Legislature but at the time still a force in the House.
So, voting in favor of casino expansion had the potential of being costly for what was McCoy’s base of power: the rural white Democrats.
Couple that with the fact that the Democratic-controlled House had been at odds with the Republican Barbour on multiple issues ranging from education funding to health care since Barbour was inaugurated in January 2004.
Barbour set records for the number of special sessions called by the governor. Those special sessions often were called to try to force the Democratic-controlled House to pass legislation it killed during the regular session.
The September 2005 special session was Barbour’s fifth of the year. For context, current Gov. Tate Reeves has called four in his nearly six years as governor.
There was little reason to expect McCoy to do Barbour’s bidding and lead the effort in the Legislature to pass his most controversial proposal: expanding casino gambling.
But when Barbour ally Lt. Gov. Amy Tuck, who presided over the Senate, refused to take up the controversial bill, Barbour was forced to turn to McCoy.
The former governor wrote about the circumstances in an essay he penned on the 20th anniversary of Hurricane Katrina for Mississippi Today Ideas.
“The Senate leadership, all Republicans, did not want to go first in passing the onshore casino law,” Barbour wrote. “So, I had to ask Speaker McCoy to allow it to come to the House floor and pass. He realized he should put the Coast and the state’s interests first. He did so, and the bill passed 61-53, with McCoy voting no.
“I will always admire Speaker McCoy, often my nemesis, for his integrity in putting the state first.”
Incidentally, former Rep. Bill Miles of Fulton, also in northeast Mississippi, was tasked by McCoy with counting, not whipping votes, to see if there was enough support in the House to pass the proposal. Not soon before the key vote, Miles said years later, he went to McCoy and told him there were more than enough votes to pass the legislation so he was voting no and broached the idea of the speaker also voting no.
It is likely that McCoy would have voted for the bill if his vote was needed.
Despite his no vote, the Biloxi Sun Herald newspaper ran a large photo of McCoy and hailed the Rienzi worm farmer as a hero for the Mississippi Gulf Coast.
This article first appeared on Mississippi Today and is republished here under a Creative Commons Attribution-NoDerivatives 4.0 International License.
The post Northeast Mississippi speaker and worm farmer played key role in Coast recovery after Hurricane Katrina appeared first on mississippitoday.org
Note: The following A.I. based commentary is not part of the original article, reproduced above, but is offered in the hopes that it will promote greater media literacy and critical thinking, by making any potential bias more visible to the reader –Staff Editor.
Political Bias Rating: Centrist
The article presents a factual and balanced account of the political dynamics surrounding Hurricane Katrina recovery efforts in Mississippi, focusing on bipartisan cooperation between Democratic and Republican leaders. It highlights the complexities of legislative decisions without overtly favoring one party or ideology, reflecting a neutral and informative tone typical of centrist reporting.
-
News from the South - Kentucky News Feed6 days ago
Lexington man accused of carjacking, firing gun during police chase faces federal firearm charge
-
The Center Square7 days ago
California mother says daughter killed herself after being transitioned by school | California
-
News from the South - Alabama News Feed6 days ago
Zaxby's Player of the Week: Dylan Jackson, Vigor WR
-
News from the South - Arkansas News Feed6 days ago
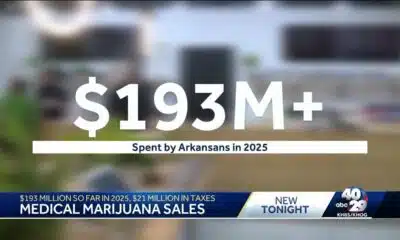
Arkansas medical marijuana sales on pace for record year
-
Local News Video6 days ago
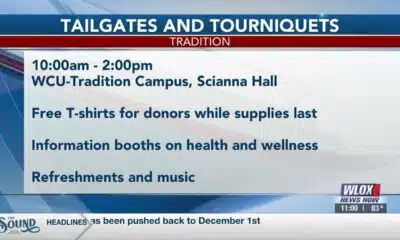
William Carey University holds 'tailgates and tourniquets' blood drive
-
News from the South - North Carolina News Feed5 days ago
What we know about Charlie Kirk shooting suspect, how he was caught
-
News from the South - Missouri News Feed6 days ago
Local, statewide officials react to Charlie Kirk death after shooting in Utah
-
Local News6 days ago
US stocks inch to more records as inflation slows and Oracle soars